Surgical Excellence with Love and Care
From Frozen to Freed, we take the gentle route of surgical relief
Today’s edition dervies from a Live Surgery performed at SOGOG’s conference. It has a little bit of everything, but most importantly, it has some love and care.
A frozen pelvis is one of the most difficult anatomical alternations that happen as a result of endometriosis. No clear planes of dissection are visible, very few lanmarks left to find the right away, and in the past, this has often been when surgeries get abandoned and an exit is made.
Fortunately, with the advancement of technology, surgical skills, and our understanding of the disease, we have a better idea of how to operate on patients having this condition.
The case we have at hand is of a 42 year old female, her intetions of fertility satisfied, and she had also previously undergone a surgery for endometriosis following which she has been on medical management for several years.
As an aside, we strongly believe that long term administration of hormonal drugs itself is a culprit of complications, often creating long term side effects for women and essentially altering the nature of tissue regrowth in endometriosis that makes dissection even more difficult when the disease gets out of hand.
You can find our full piece on the downsides of medical management by clickin on this text here
That being said, let’s move back into the surgery.
Dealing with difficult cases of the frozen pelvis means we have to follow a slow and meticulous process of dissection throughout the surgery. We must treat every step as crucial and important, every fibre cut, every tissue dissected must be taken seriously, and after consideration.
This of course doesn’t mean we hesitate, but that we remain fully present, and aware of what we are doing. That’s the only way we can incrementally move towards surgical excellence. This method was long ago articulated as The Mathematics of DIE Surgeries where a clear aim, with the right method, and wisdom put together over the years, mitigated with the risk involved and finally made complete with a sense of excellence leads to the best surgeries.
We begin in this case with the first step of Colon Mobilization
Beginning from the left lateral brim of the pelvis, we conduct the most important step of the surgery: sigmoid colon mobilisation. Important because mobilising the colon is the easiest way to unravel the pelvis. It is an important anatomical marker that isn’t distorted too easily and often marks the outer edge of how far the disease might have spread.
And more importantly, this gives us the space and exposure required to conduct further dissection in the pelvis.
Identification of ureter on the left followed by ureteric dissection
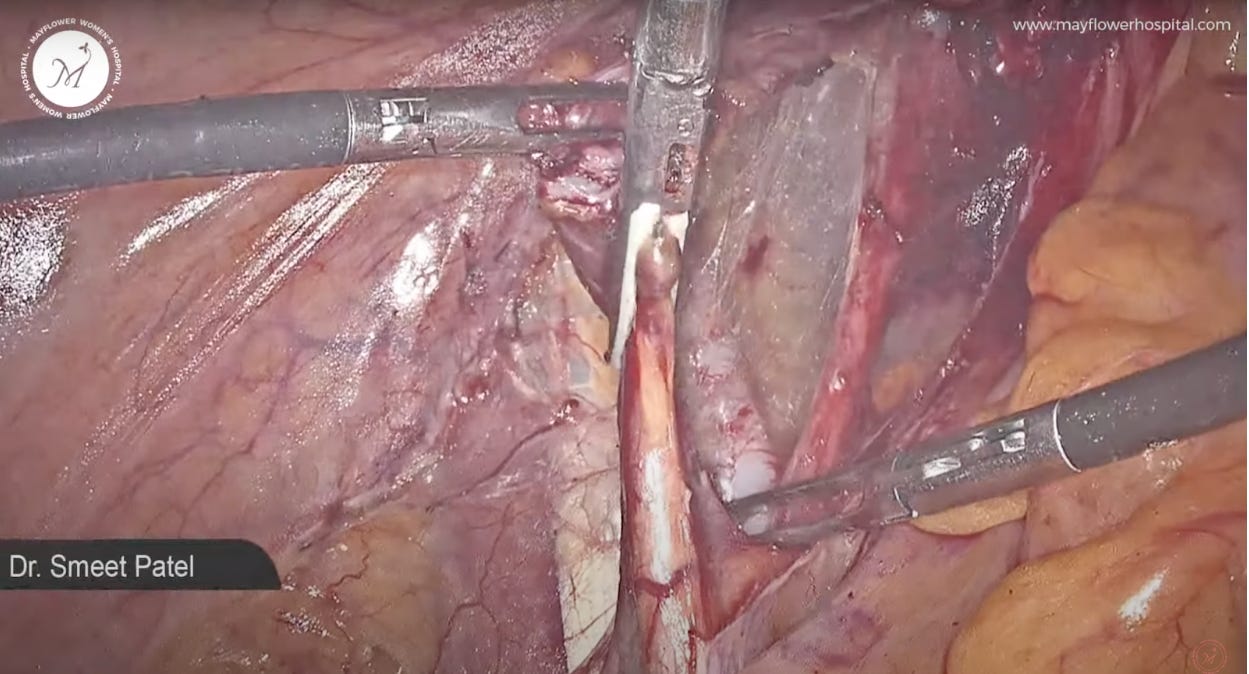
Now with proper traction and counter traction we identify the ureter and ureterolysis is performed preserving the myssentry of the ureter while using slow and steady fibre by fibre dissection to denude and free the ureter from any surface effects of tissue growth.
We stay on the anterior surface of ureter and dissect parallel to ureter till we reach the end point.
On a case to case basis, Uretrolysis can really vary and often prove to be very difficult. We documented our findings and methods in an issue titled The 5 Levels of Ureteric Dissection that you can read here
Left Tubo-Overian Mass Excision
Next, we proceed towards the removal of the left Tubo-Ovarian mass. Remember the cytoreductive surgical approach - it helps us in removal of plaques and masses. Once done, we move further with our dissection; now with better vision and without disturbances.
In the next step we skeletonize the IP ligament and make a window between the ligament and the ureter, following which we coagulate the ligament, and cut.
We then repeat a similar procedure on the other side as well. We are slowly getting closer to an anatomical restoration of the pelvis. Up next is one of the most important steps in that process.
J Curve Dissection
Now we move on to declutter the pelvis, and restore normal anatomy in the pouch of douglas, just at the clutterment of the tauras-uterinus area. While continuing with our ureterolysis we dissect in a J shape towards the medial side. This step helps in opening of pouch of douglas and creates room for us to continue dissection.
Vascular Web Dissection and Removal of Parametrial Nodules
Next, we enter into the retroperitoneal area performing fiber by fiber dissection. In line, we skeletonize the uterine artery and coagulate it. We also carefully (and with love) remove the nodules over the internal iliac tree branches. This typically is a presentation of parametrial involvement of the disease and we perform the removal along the vessels.
We say with love and care because at this point it becomes very important to understand that leaving behind any large incidences of the disease can, and most certainly will, result in recurrance of the disease. Symptomatic recurrence might happen a little later and often in worse ways than before but the disease has a way of coming back, unless we conduct a total removal.
This is also what has pushed surgeons at Mayflower to find every possible method available to us to dissect a disease and remove even the small inclusions in the tissue. Deep infiltrating endometriosis really does go deep.
Medial Pararectal Space Dissection and a Nerve Sparring Surgery
We enter into the medial pararectal space, dissect fiber by fiber and make sure that the fat always falls to the rectum. This means that the outer margin of the fat, away from the rectum will define our plane of dissection, while the mesocolonic fat stays with the rectum.
In the process we also make sure that the hypogastric nerve is not injured and completely preserved along with its small nervation into the colon. This care will help to a great degree in post op recovery of the patient.
The Rule of M
Approaching the colon, we now start to notice all the sites of disease involvement. To deal with it, we first dissect the fat surrounding the endo plaque on the colon.
The nodule is held firmly and a fiber by fiber dissection is carried out.
The nodule here does not infiltrate the muscularis (innermost) layer of the colon. That can be typically found out right from an MRI scan done after proper patient preparation. Since it doesn’t infiltrate too deep, and is a single localised nodule covering less than 30% of the cirrcumferrential area of the colon, we know that this is a case of rectal shaving.
You can read more about The Rule of M in our video publication here
We shave off the nodule from the colon, maintaining the integrity of colon and hence resulting in lower morbidity, faster recovery, and great compliance from the patient.
The rent is sutured in a single layer with barbed suture 3/0 in a continuous non locking fashion.
When we started, we entered into a frozen pelvis, with no possible way of getting in or even seeing the damage the disease had done. On the other side of this surgery, anatomical restoration is done, we have removed all the endo nodules/plaques, performed a laparoscopic hysterectomy and Voila! we have a neat and clean pelvis.
No disease, no endometriosis, no pain, and a very good quality of life awaits her outside this OR.
That’s all!
Hope you’re back from your year end vacations and getting your hands dirty already!
And while you’re at it, registration for our 13th bactch of CSEEMIG, a 4 day program of intensive in-OT learnings combined with an excellent series of lectures, is LIVE NOW!
You can register for the workshop here —>
It begins on Jan 21st, and ends on 24th where a small group of like minded high functioning and very smart gynecologists will join you in the process of learning. Come down! You might even make a friend or two, besides of course learning so much more than I can type in this newsletter.
That’s it for this week! See you soon!