For our long time readers, today is special. This is the first Endometriosis Weekly Video Edition. This week, you can not only read but click on the video above and watch the surgery we’re talking about.
If you’re reading this edition in your email, I strongly suggest you click through and watch the video as you read along. Alright, let’s get on with it.
There is a gaping hole at the centre of how treat endometriosis of the colon.
There has been a recent surge in the number of cases that undergo a resection procedure following endometriosis of the colon. “So What?” You could ask. There has been a rise in surgeries for endometriosis in general. Isn’t that a good thing?
Not necessarily.
Surgery isn’t something the body is expecting and preparing for, let alone a radicle procedure like resection.
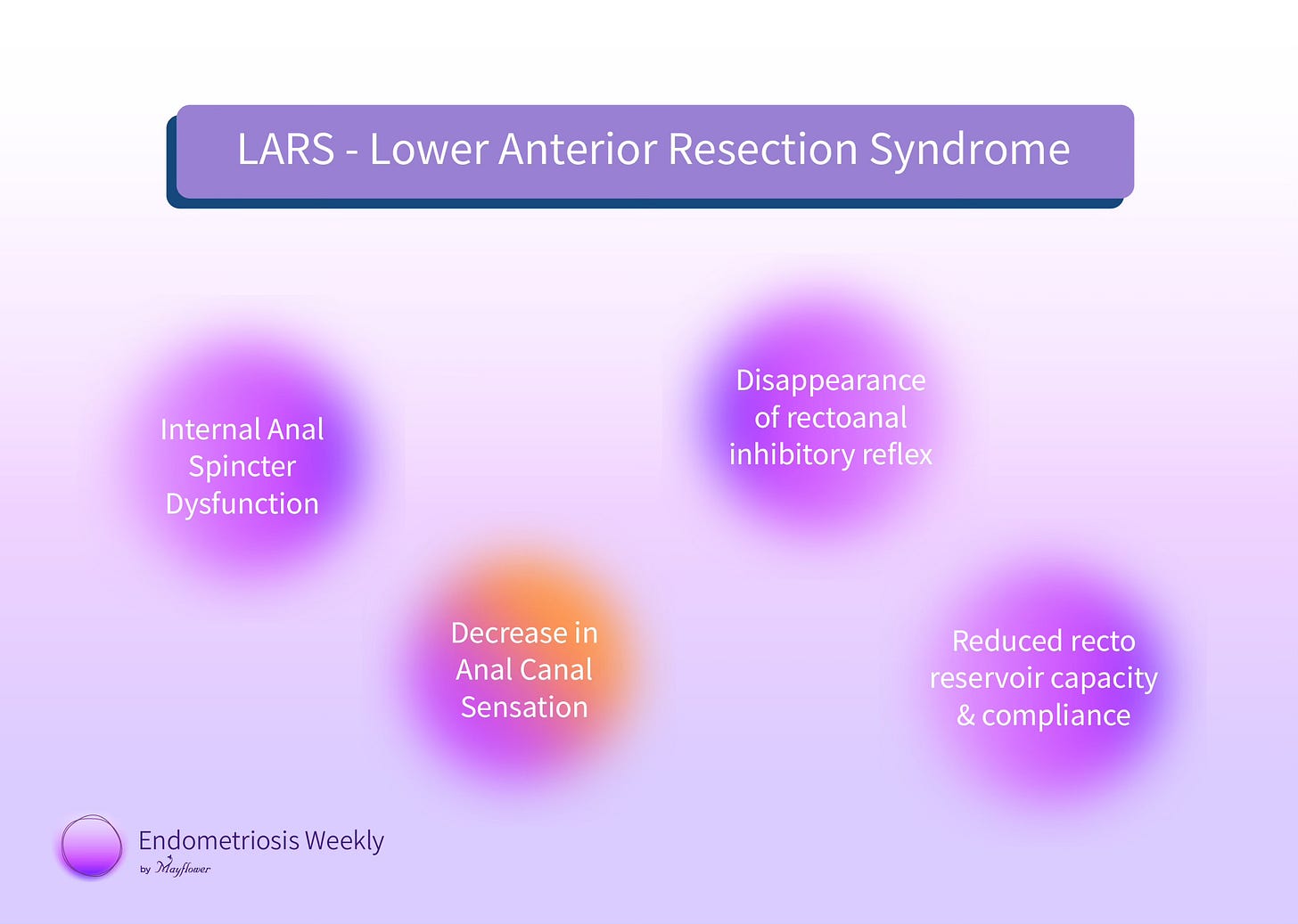
A premature decision to conduct a resection procedure can also result in LARS, or the Lower Anterior Resection Syndrome which can make the cure more painful than the disease for a patient. LARS is often silently mentioned in consent printouts with neither the patient nor the doctor fully understanding the extent of its impact.
The LAR syndrome is likely multifactorial and several proposed pathophysiological mechanisms for LARS include internal anal sphincter dysfunction, a decrease in anal canal sensation, disappearance of recto-anal inhibitory reflex, and a reduction in recto reservoir capacity and compliance. As a result, patients suffer from grave post-op recovery periods and suffer a great deal more emotionally.
After seeing the outcomes of LARS first hand, we at Mayflower knew that we just had to find a better way of doing this. If we could somehow evade the procedure of resection altogether, take a more conservative but tailor made approach, that would still result in a total removal of the disease, we would be able to bring down the incidences of LARS.
We began by thinking; instead of dissecting the full circumference of the colon, we only needed to dissect as much as needed, with minimal disturbance to
The neuromuscular continuity of the colon
The luminal diameter available for stool to pass
The first principles at play here are surprisingly simple. If we avoid R&A, we avoid complete discontinuity. Even if we need to suture it back after an anterior discoid resection, it will adapt to the new lumen available. Given the circumferential involvement is limited.
That’s when we developed The Rule of M.
We started to look at the edge cases. Instances where one could manage with shaving or anterior discoid resection (ADR), but where resection just also have been an option, and we started to better classify these.
Let’s break this down into different cases. One step at a time.
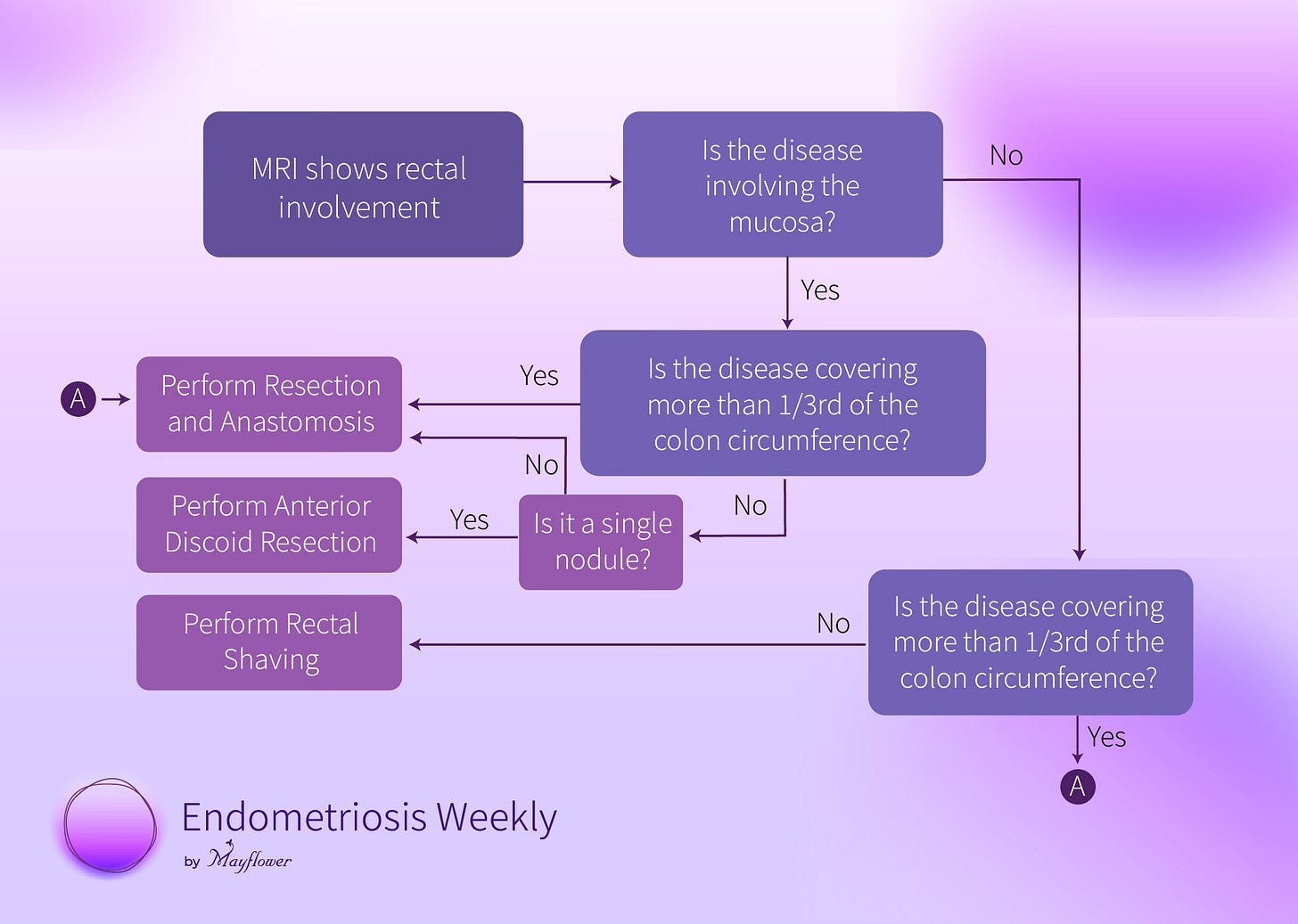
First, we had the localised extra mucosal nodules. Meaning, that they cover less than a third of the circumference of the colon, and aren’t invading the mucosa of the colon.
That last bit, about not invading the mucosa, that’s important. The mucosa directly represents the available lumen of the colon and any invasion to it, means a dissection will reduce the finally available lumen at the point of repair.
Next, came the localised nodules (covering less than a third of the circumference of the colon) that were invading the mucosa. This required that we excise the full nodule. If it’s a single nodule, this could’ve be achieved via an anterior disc excision. Here the lumen would directly decrease but the flexibility of the colon makes things easy.
If we have multiple nodules, resection is the only way.
Finally comes the case where circumferential involvement is more than a third of the way around the colon. In this case, regardless of whether the mucosa is involved or not, only shaving off the nodule and suturing it back will cause significant bunching up of the internal lumen effectively reducing the net available area and crossing the threshold of what the colon can compensate for. Which is why we prefer a resection and anastomosis procedure.
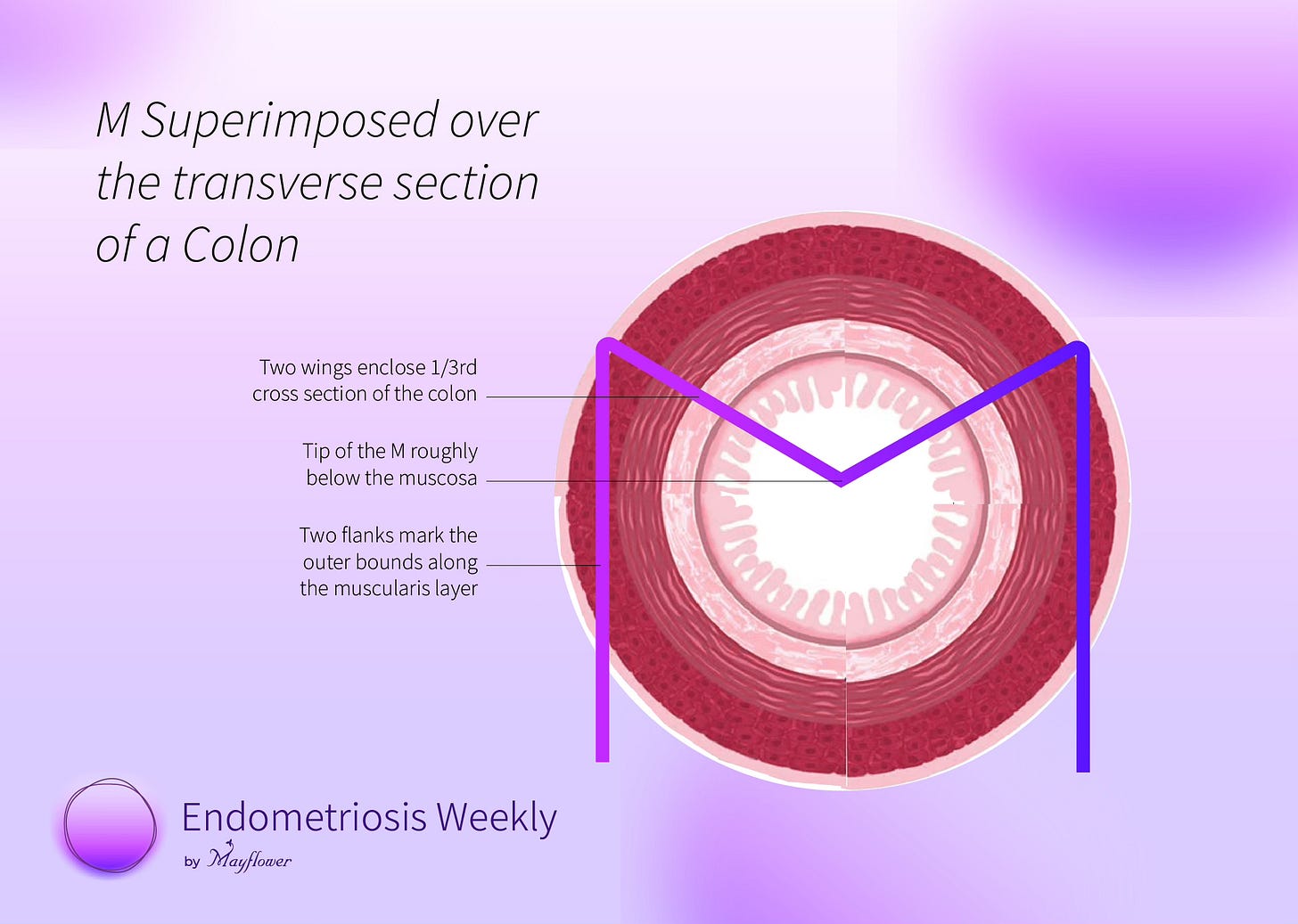
To make this simple, we made a visual guide that we call The Rule of M
Imagine the cross-section of the colon, and superimpose an M on it.
The two legs of the M mark the outer bounds of the colon while the two wings of M mark between them a 1/3rd section of the colon, with the tip of the M falling roughly where mucosa ends.
If the nodule(s) fit within the two wings of M and isn’t invading the mucosa, perform rectal shaving. This will cause minimum damage to the continuity of the colon and protect nearly the entirety of its luminal area previously available.
If the nodule is single, fits within the two wings of the M, but is touching the tip (invading the mucosa) it’s a case for anterior discoid resection (ADR). If they’re multiple, choose resection and anastomosis (R&A).
In case the nodule crosses over the two wings of the M, go for R&A
Note that the length of the colon involved is not at all of concern here. At Mayflower, we’ve shaved significant lengths of the colon with this thumb rule seeing no change in patient outcome and pain relief or hospital time post-surgery.
For the engineer inside you, here’s a flow chart.
It’s that simple.
With this, we’ve been able to triage several patients who were declared candidates for R&A into a more relaxed group of shaving and ADE candidates.
The video covers in detail the steps involved in this procedure. We would love to know what you think of it and how you approach the problem of colonic endometriosis.
Until next time!








Share this post