GnRH regulators are Endo's newest friends in town
Rampant medical management of endometriosis is setting up thousands of Thousands of women for eventual suffering
There is no fancy way of saying this, so let’s just say it right at the top. Medical management of endometriosis for extended periods with the use of GnRH agonists and antagonists is a highly counterproductive exercise and is worseing the indensible surgical outcome on the other side.
Today, we will use an empherical understanding of the growth of the tissue, coupled with surgical images and observations to break down exactly what goes wrong when a person with endometriosis is put on medical management for a long time.
Endometriosis is a benign disease. But it behaves quite malignantly.
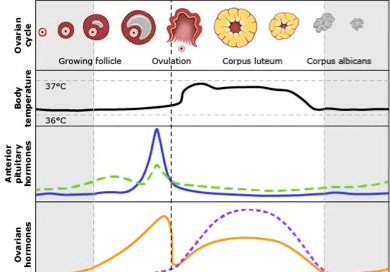
Take the simple process of menstruation. The hypothalamus releases Gonadotropin Releasing Hormone (GnRH) which gets the Pituitary gland to release the Luteinizing Hormone (LH) and the Follicle Stimulating Hormone (FSH).
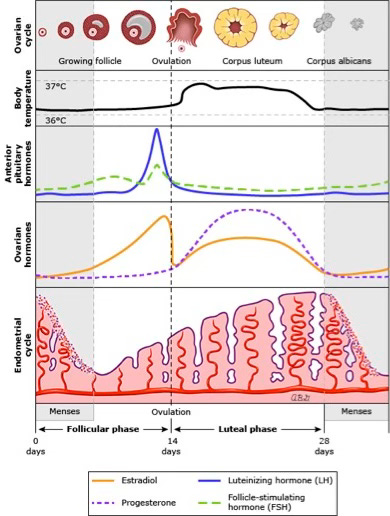
These then propagate the ovaries to produce Estrogen and Progesterone in an intricate dance that forms the basis of all human life. Endoemtriotic cells in ectopic sites across the pelvis react to these hormones differently. We’ve observed that they still follow a cycle of layer by layer growth and shedding but with added variables.
The cycle of growth —> shedding is followed closely by fibrosis since these ectopic tissues have no specific exit pathways.
Stuck now between a rock and a hard place, this tissue is attacked by the body’s own immunity, which realizes it isn’t foreign material and chooses to fibrose this mass in place. Which is a great mechanism to deal with extra tissue, if that’s all it was. But it isn’t.
As the days go by and FSH level rises again, this fibrosed site is now a new location for cell growth. The cycle starts again. There’s tissue growth around the new seed, there’s shedding at the end of a cycle, and that’s followed by fibrosis.
So far so good. Once the fibrosed nodule has grown big enough to cause trouble, mostly as abdominal pain, the patient reaches out to a doctor who observes this growth, and in several cases chooses to begin medical management with GnRH agonists and antagonists.
Without getting into the mechanism, it suffices to understand that these drugs downregulate LH and FSH, subsequently halting menstruation. However, the effect of the drug isn’t curative at all. All it can do is hold the growth of the disease for a few cycles and cause a small reduction in the nodule size. But that’s about it.
And not for long.
Once the effect of these drugs vanes off, we observe an immediate surge back, of growth, shedding, and fibrosis. In come the hormones, with them the abundance of growth, and shortly after, the excruciating pain.
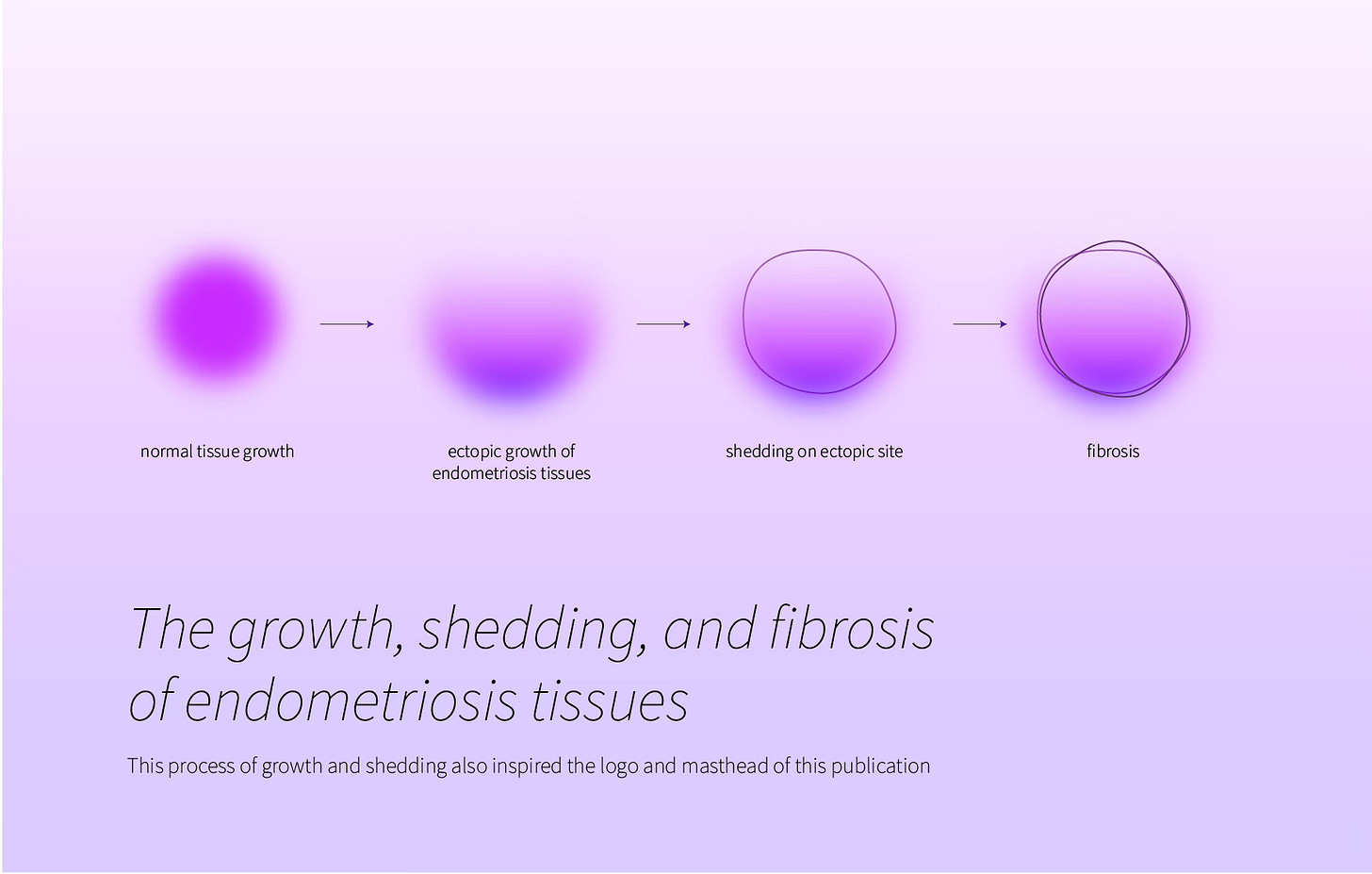
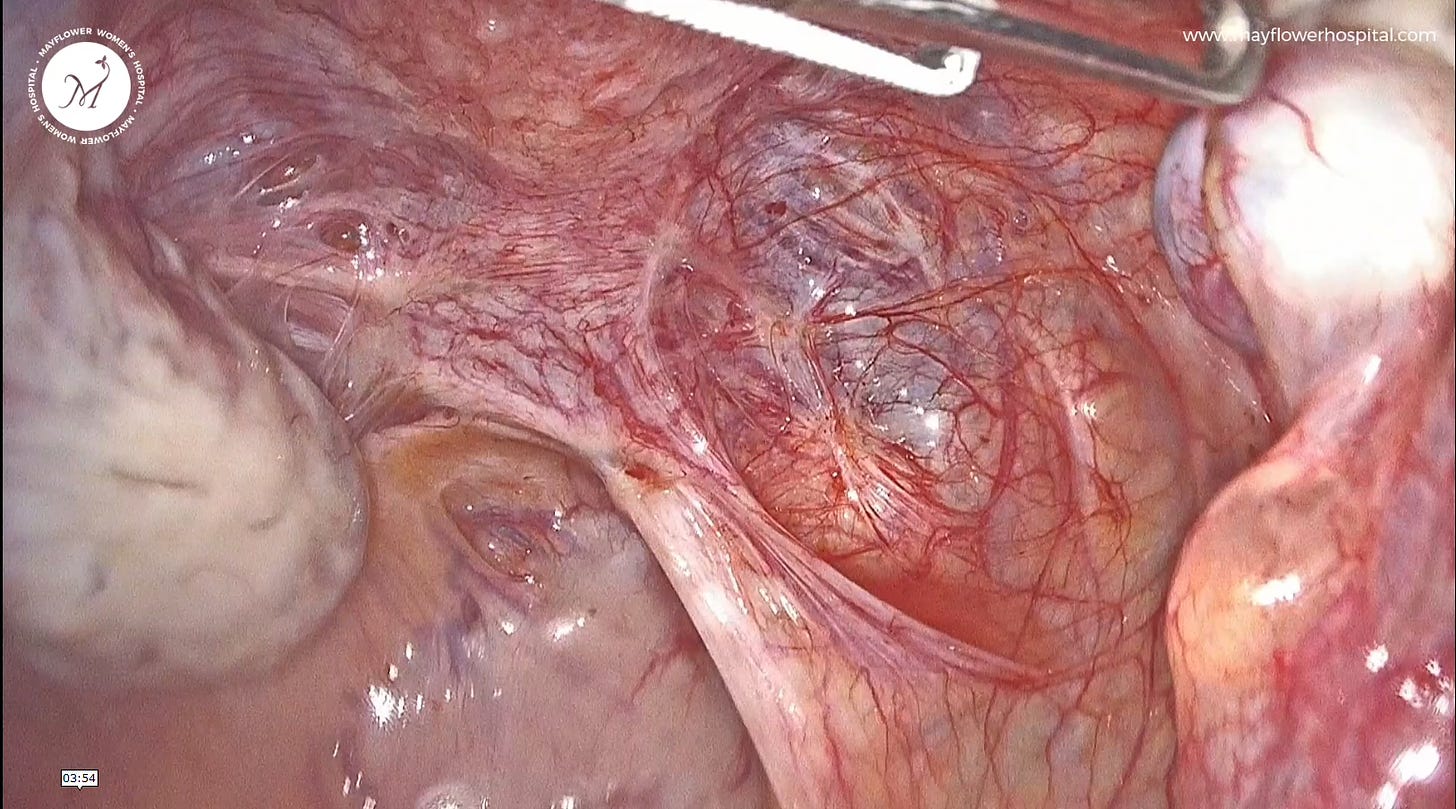
This time, when surgery is looked at as a solution, we have some damning observations to share. Patients who have been on GnRH regulators for too long, , or any kind of medical management for that matter, present nodules with no clear planes of dissection. They’re limited in size but very challenging to remove.
When growing under the influence of the natural cyclical secretions of FSH and LH, these nodules grow layer on layer. So dissecting them is easy.
But when kept away from this layer by layer growth and shedding, the nodule turns near amorphous, making it very hard to secure a clean line of dissection. We wrote a thesis on the types of tissues found during the surgical management of endometriosis. You can read it here. For the purpose of this edition, we highlight a specific tissue called The Poison Pill.
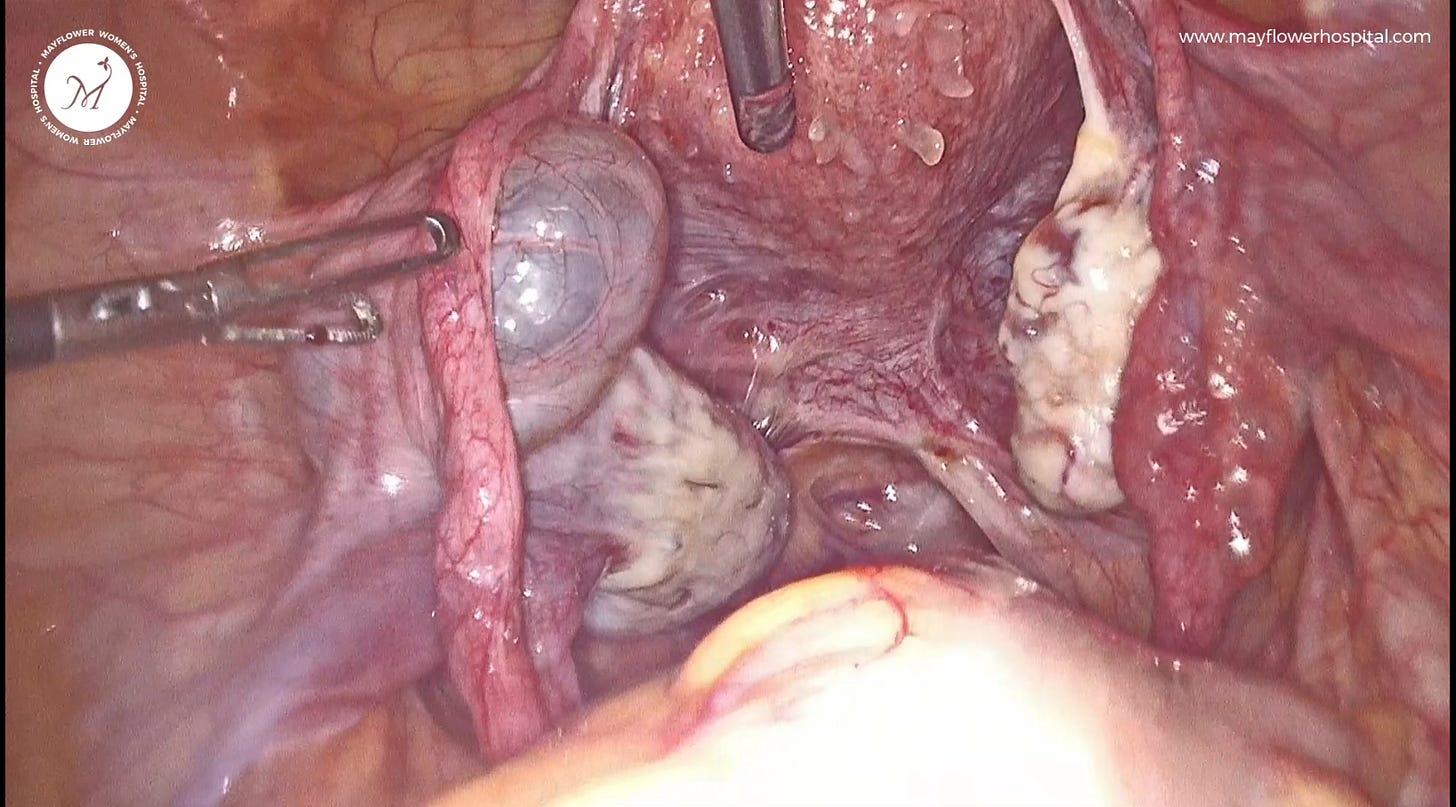
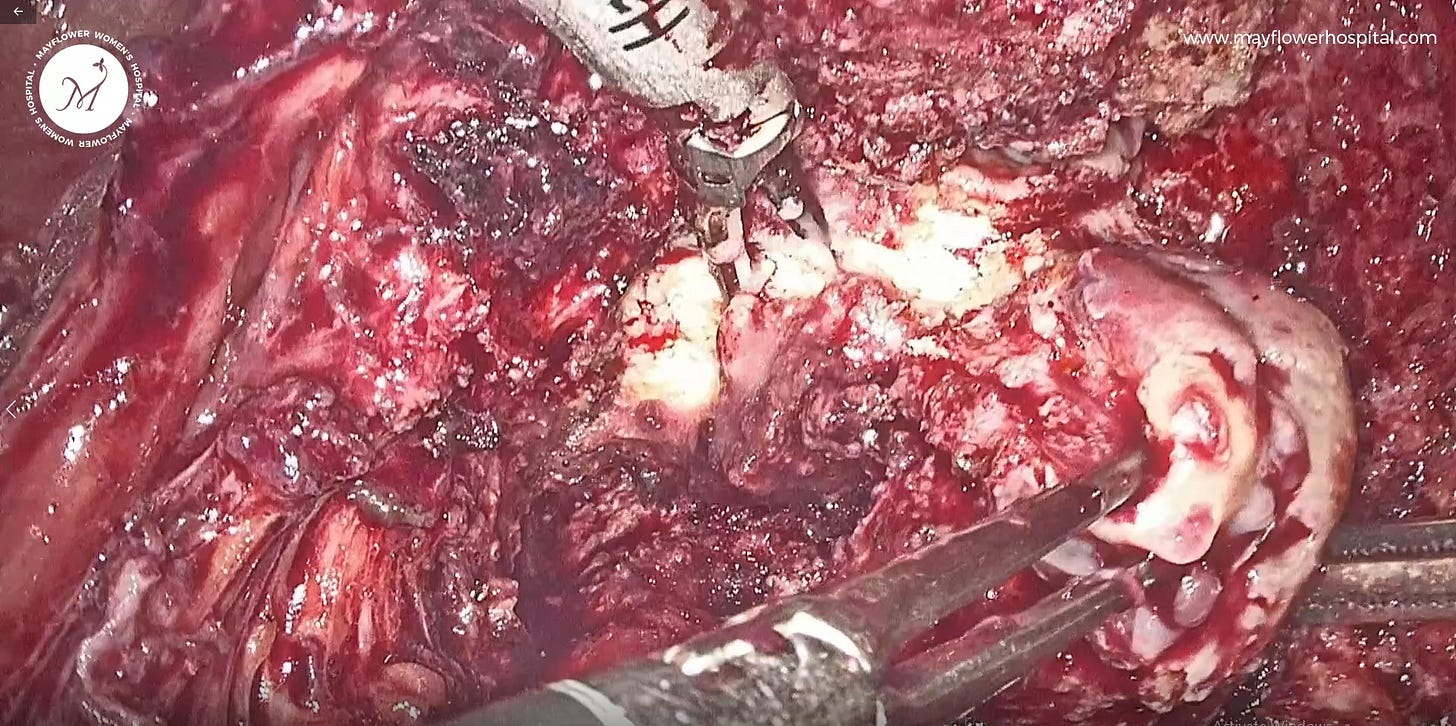
These endometriosis tissues turn into thick, rubbery, dense masses with no clear planes of dissection. What’s seen below is the presentation of a nodule in a patient who had been administered GnRH agonists for 3+ years following an incomplete surgery for endometriosis. Here’s an example from another case we have observed
And while we’re drawn to think that the drug is the problem, it’s important to change how we look at the problem; how we approach a prescription, and what makes for the right nature of prescription.
Historically, and understandably, surgery has been thought of as a progressive step to medicine.
Patients too, for reasons well understood and only rational, prefer to begin with medical management first and therefore consider surgery as a progressive step to the failure of medication. But when dealing with endometriosis, we are presented with a unique challenge.
Surgery here isn’t the next step to medical management, it’s an alternative from the very beginning. It’s counterintuitive, more for patients than doctors, but over several years and thousands of surgeries, we’ve observed this to be true.
It is possible that some time in the future, medications relevant and effective enough emerge that are able to curb the disease altogether. However till then, our only source of truth is what we see. And what we see is not nice.