The Correct Use of Medical Management in Endometriosis
ME Protocol - leveraging pregnancy for reduced recurrence
Mayflower’s guiding principle in treating endometriosis can simply be stated as
“A surgery begins long before the scalpel first touches the skin, and lasts long after the last suture has dissolved”
Surgery begins with how you introduce your patient to the idea of the disease itself, how you choose to diagnose it, what treatment options you decide based on that diagnosis; that’s the before part. But what happens after? What do we really mean when we say a surgery lasts long after the last suture has dissolve?
In today’s edition of Endometriosis Weekly, we look at maternity, an unlikely partner to surgery, and how it can help significantly reduce the risk of recurrence in post op Endometriosis.
The ME Protocol
Short for the Mayflower Endometriosis Protocol for Fertility Intent in Endometriosis, ME Protocol was developed with an intent to see how far we can go in achieving a complete removal of the disease.
This protocol has four primary steps
Total and restorative fertility preserving and enhancing surgery
Clinically induced amenorrhea
Fertility planning - natural + assissted
Gestational and lactational amenorrhea
Let’s look at the significance each step has in the process
Total and restorative fertility preserving and enhancing surgery
We’ve written quite extensively about recurrence reducing procedures in our previous editions. While the Mayflower Butterfly Peritonectomy is exclusively focused on reducing recurrence, the Sanjay Patel Classification of Adenomyosis and its related procedures, together with the Five Levels of Ureteric Dissection help in anatomical restoration.
The goal is get as much of the disease out as possible, from as many places as it might be present while preserving and/or enhancing the fertility prospect of the patient. The only tissues left behind are microscopic implants that are imperceptible both to the human eye and to conventional MRI.
Clinically induced amenorrhea - 6 months
This is followed by a clinically induced amenorrhea. We practice giving Leuprolide post recovery from surgery since it’s a single shot injectable that leads to ~6 months of amenorrhea, however side effects considered, some cases fare better with a Dienogest 2mg prescription.
This practice gives the body time to recover and recuperate from the trauma of surgery at sites that were earlier highly active through the ups and downs of hormones in any given month.
Loosely speaking almost 75% of the recovery happens in the first three months. For this period, it’s ideal to keep any hormonal undulances at bay. The GnRH analogues mentioned previously help down regulate hormones and keep things mellow.
Fertility Planning - Natural + Assisted - 3 months
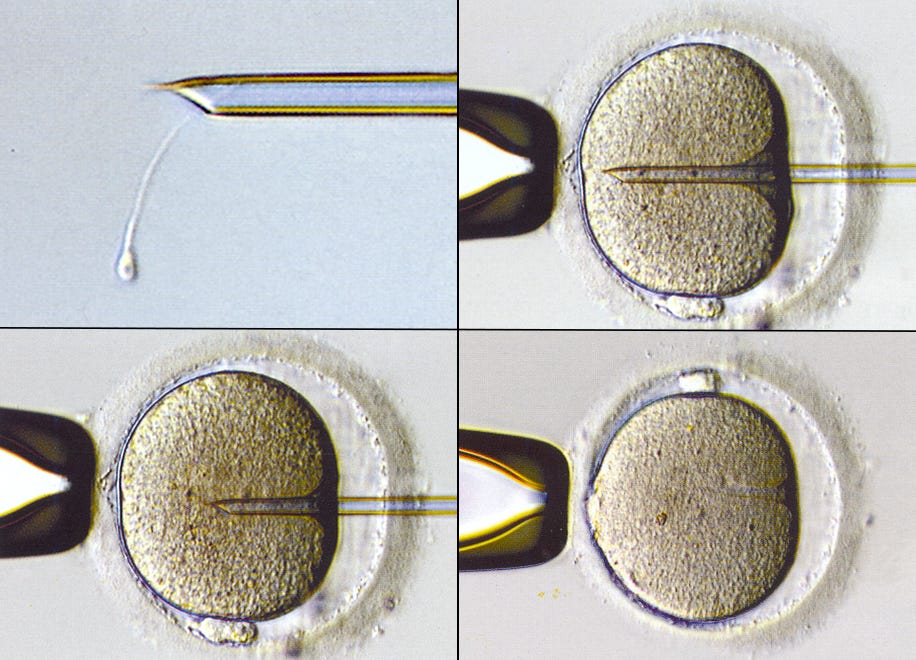
We typically counsel couples open to considering pregnancy to begin trying for conception immediately after the natural cycle resumes. We typically give them three months to attempt a natural pregnancy. If it is already known that the likelihood of a natural pregnancy is low, they may be advised to go for IVF.
Either way, conception is pursued.
In an observation of 617 patients of fertility enhancing endometriosis surgeries between 2019 and 2021, it was found that 45% were able to conceive naturally after surgery. This was possible because of a complete surgery with steps including complete removal of endometriotic cysts from ovaries (not simply drain them), reestablishment of a good tube-ovarian relationship, and other procedures that enhance and preserve fertility.
Of the 55% unable to conceive naturally, 42% were able to conceive in the first cycle of IVF and subsequently another 32% conceived upto the third cycle.
Gestational and Lactational Amenorrhea - 22 months
A successful pregnancy further leads to 9 months of gestational and 12 months of lactational amenorrhea. This we believe is the strongest agent of recovery. All the microscopic implants that were inadvertently left behind in surgery, the seeds of future recurrence, spend almost 30 months with little hormonal concentration to induce growth.
In this 27 month period, it is likely that the body’s immune system recognises the ectopic nature of these tissues and causes apoptosis over a period of time, rendering them incapable of growth once the hormones come back.
The ME Protocol put together with our data on radical surgeries has given us a net recurrence of 1.8% against a global average of 40+%
It is likely that more than one factor is at play in reducing recurrence, but we are significantly convinced that pregnancy has a big role to play there.
One of the key limitations, as you might already have guessed, is that this does not apply to patients who simply don’t want to pursue pregnancy or are beyond the point where they can. A total and restorative surgery, followed by a clinically induced amenorrhea is still an option available to them, an option that also provides a significant hormone free period for the body to recover.
In closing, we would like to go back to what we started with. “A surgery begins long before the scalpel first touches the skin, and lasts long after the last suture has dissolved” Now we know how a surgery lasts long after the last suture has dissolved.











Intresting read!! ❤️