Managing Deep Bladder Involvement in Endometriosis
A procedural walkthrough of exactly how much you need to know
We had a lot of fun writing about the mechanic and the surgeon last week. Looks like a lot of you enjoyed it too. We love reading your email replies so keep them coming!
In continuation of the theme, we figured that it would be best to share with you the next level of disease involvement of the bladder.
Mucosal involvement of the bladder in cases of deep infiltrating endometriosis often shows up as very bothersome and life-hindering symptoms. While a direct symptom-to-occurrence causation/correlation isn’t established, sometime back we published an edition called “The Unofficial Symptom Map of Endometriosis” which talks about symptoms that might be signs of bladder endometriosis.
Urinary frequency, Urgency, and/or Painful Micturition
Bladder endometriosis typically presents with nonspecific urinary symptoms of frequency, urgency, and pain at micturition. This symptom set can worsen with menses. However, ureteral endometriosis can be asymptomatic or at best associated with colicky flank pain or gross hematuria. This makes ureter a silent victim of endometriosis and it’s often very late by the time people find out about it.
Why talk about symptoms if we don’t have a conclusive correlation?
A person suffering from endometriosis may or may not see a gynaecologist when their symptoms are renal troubles. There’s that old radiology dictum, “If you’re not looking for it, you will miss it” And that often happens in cases where endometriosis is not in the specialist’s consideration at all.
Fortunately, as the years go by, more and more specialities, specifically gastroenterology and urology are becoming more aware of the presence of this disease. Even then, mapping it becomes crucial to finding the next steps of surgery.
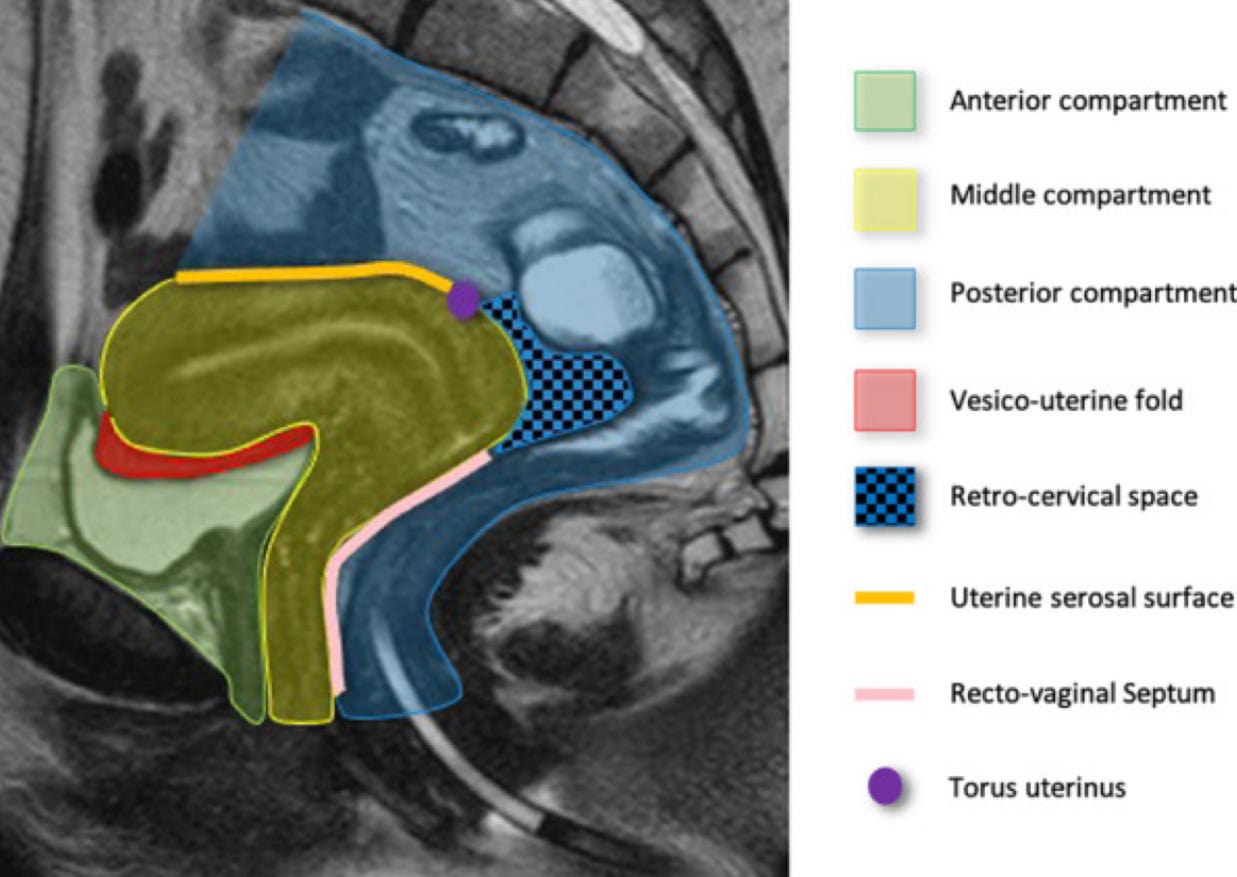
Bladder Endometriosis shows up in the anterior compartment in our MRI
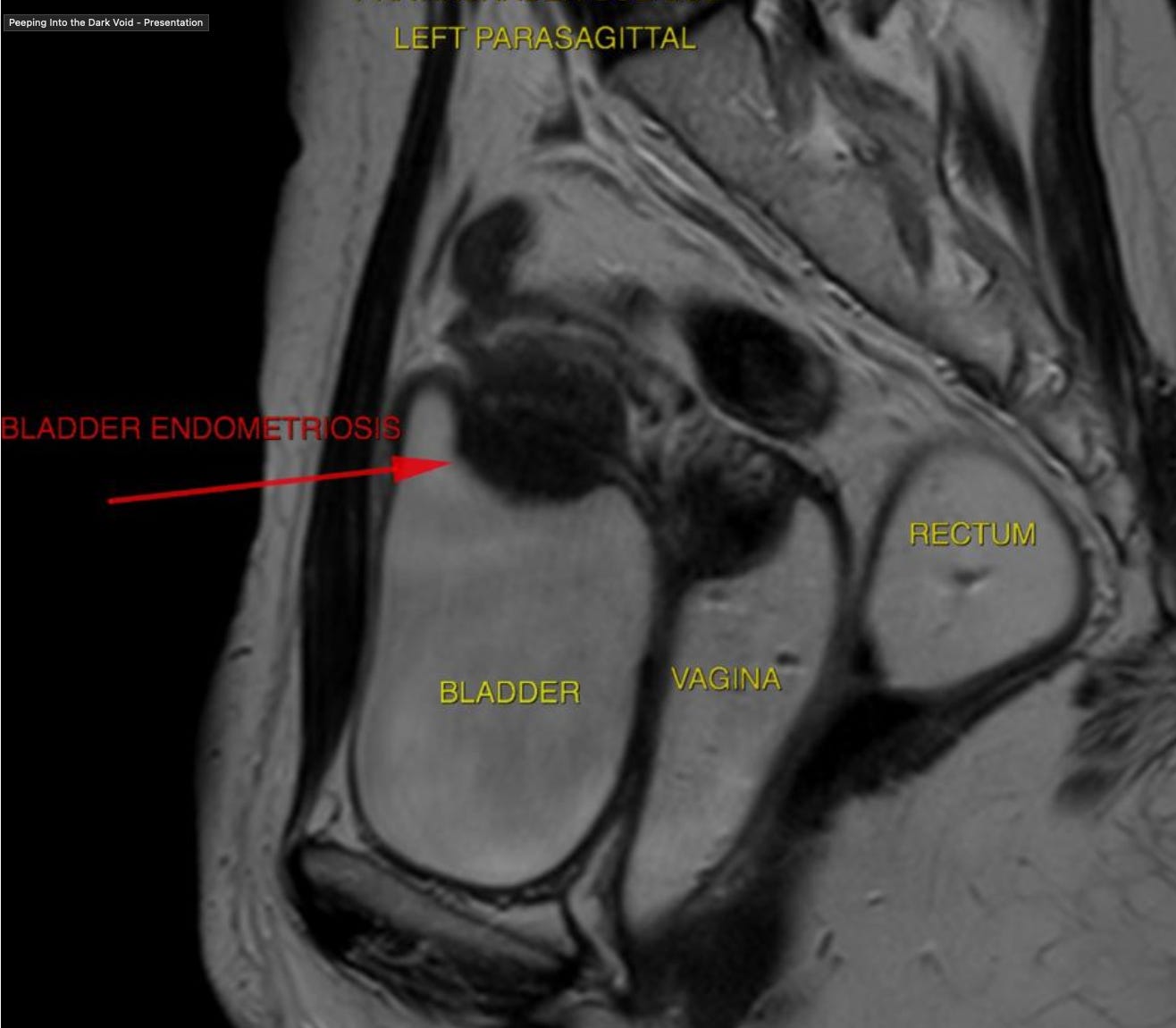
When involved, it looks something like this
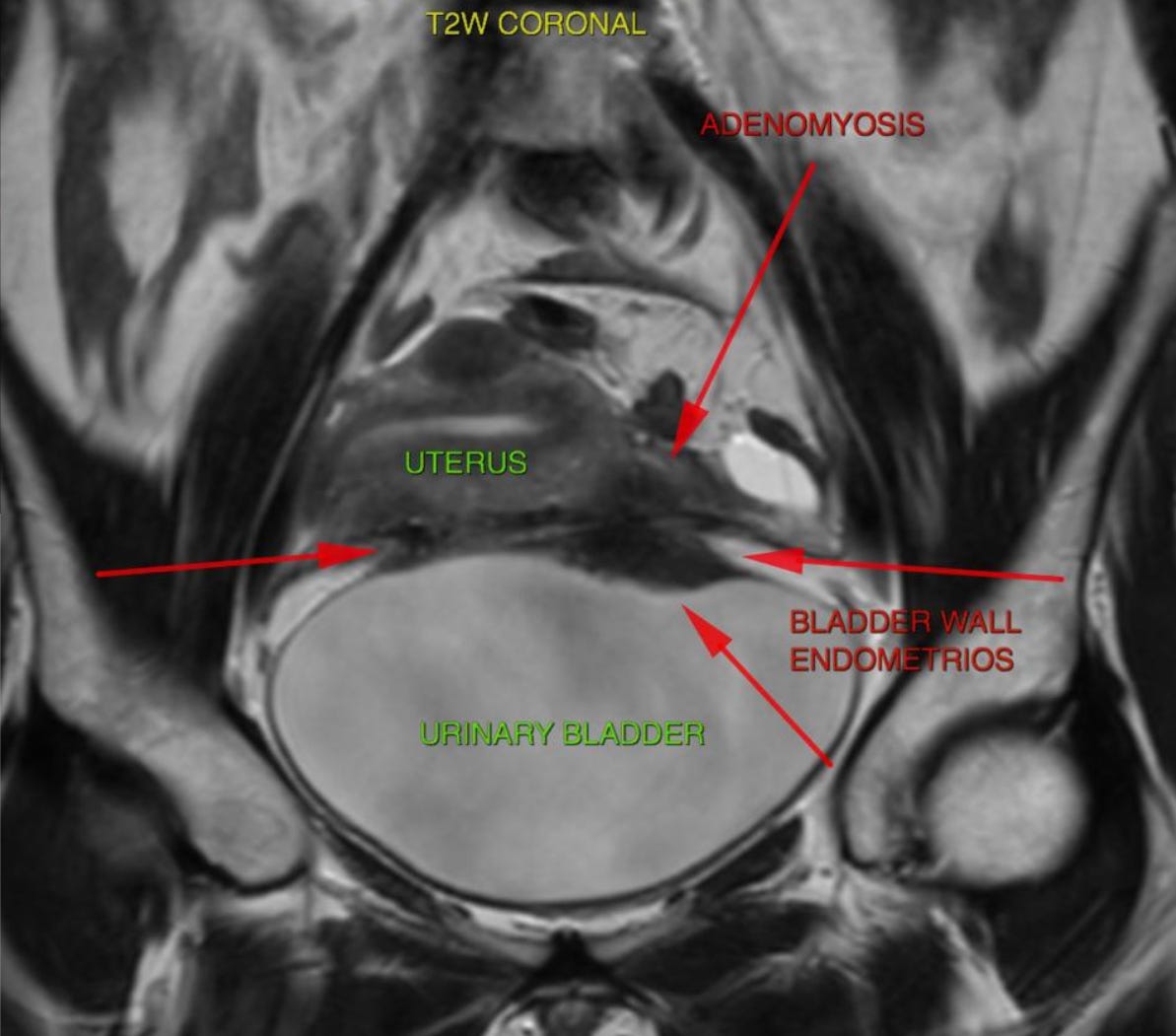
Here’s a similar nodule from a different plane. This is along the coronal plane.
Mapping well is the first step to preparing for a successful surgery. Pro tip: Make sure your radiologist reports for:
Lesion Size and Location
Depth of detrusor muscle invasion
And distance from UVJ (Uterovesical Junction)
While the rest of this edition might talk about the surgical management of the disease, do not for a moment consider the management of this case as a surgical only. A successful treatment involves restoration of life, not just the disease and therefore several people, very good with their jobs have to come together in order to make a treatment successful. At Mayflower, this typically involves
Me as an endo surgeon
Gi surgeon
Uro surgeon
A team of anesthesiologists
OT/OR assistant team
A team of residents and fellows
Medical officers
Councillors
An involved perioperative care unit
Team of physicians
Nursing team
Only with the right ecosystem are we truly able to put together the treatment that our patients deserve.
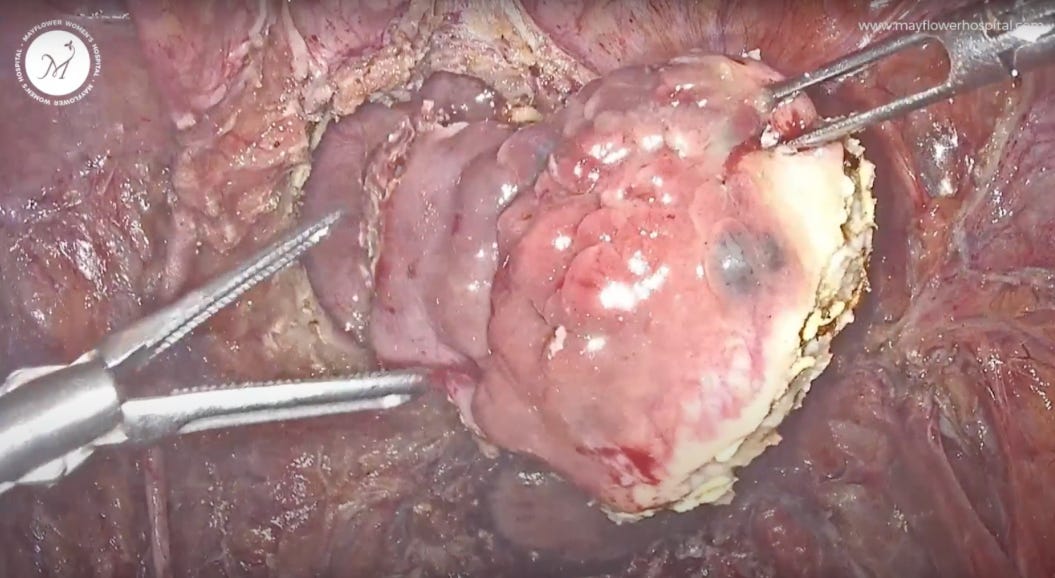
Alright, let’s jump in now. Once we’ve mapped the disease, we must confirm it. Surgery begins with a cystoscopic view from inside the bladder where we mark the disease.
The ureteric orifice and trigone area appear normal but we can see some endometriosis plaque buildup involving the mucosa on the dome of the bladder.
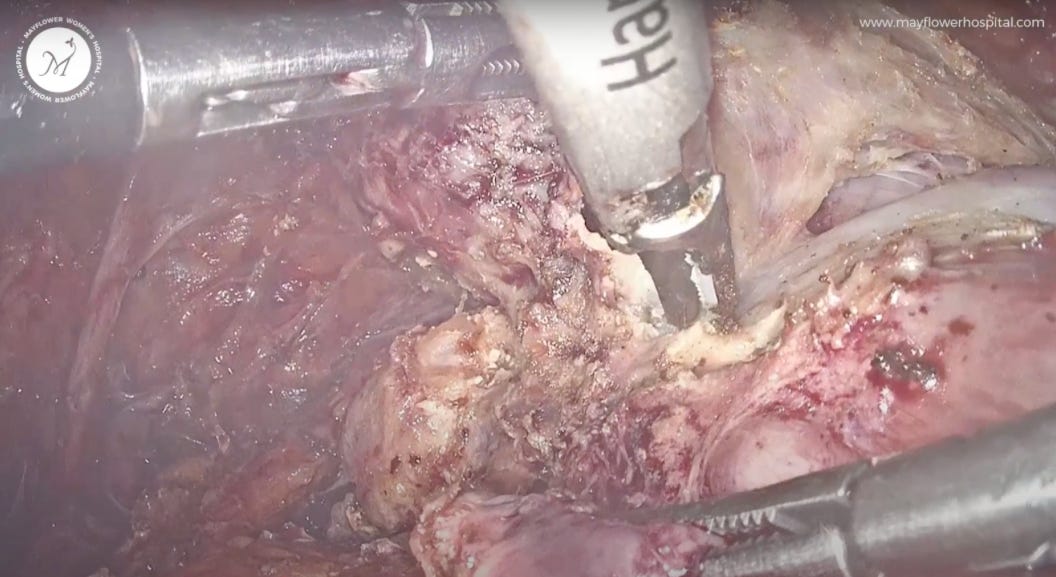
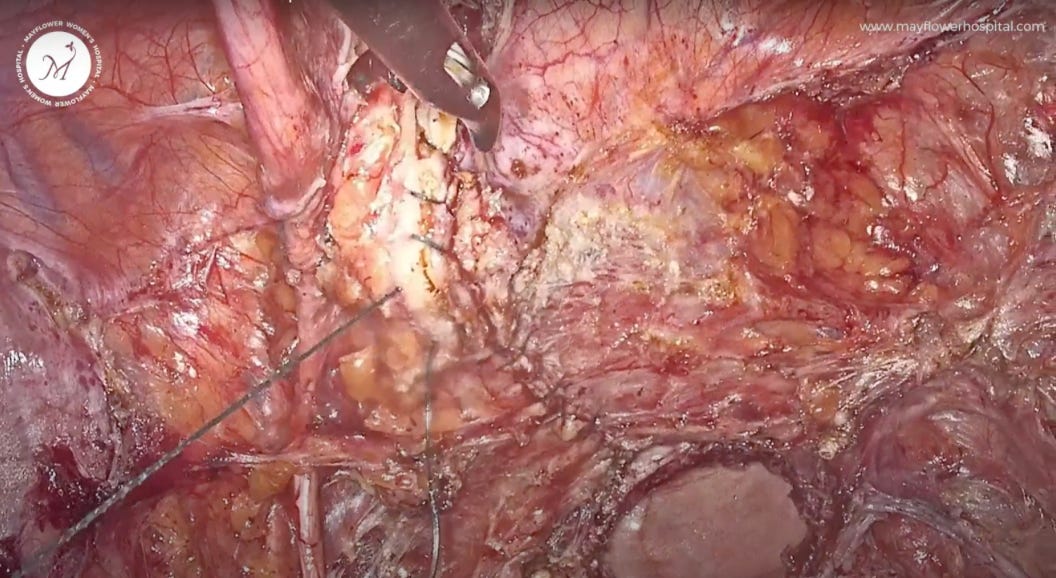
Laparoscopically, we first remove all the various diseased instances of endometriosis from within the pelvis and then focus on the bladder.
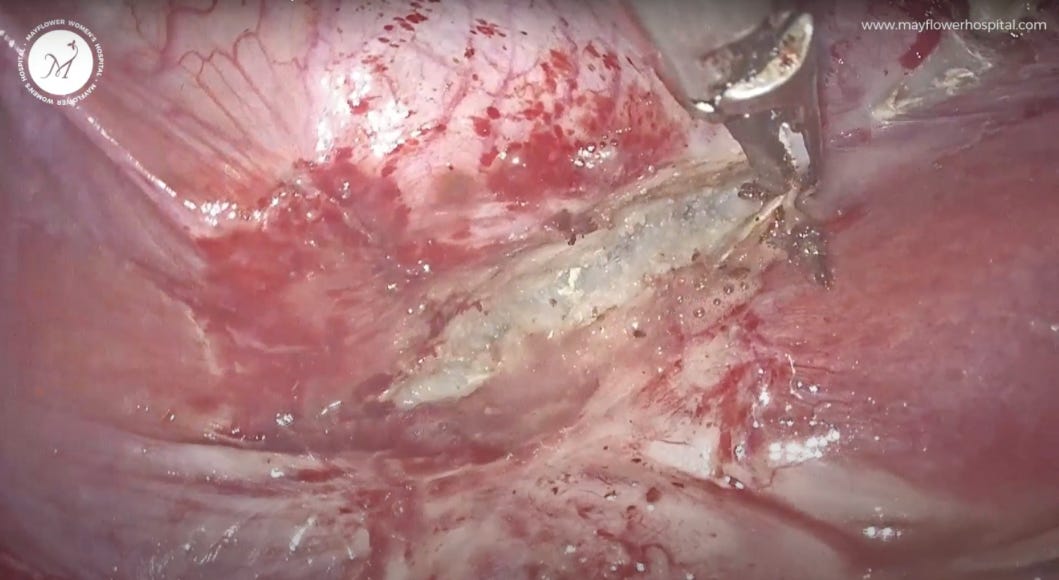
The fundamentals of dissection are the same as we discussed in the last edition : The only thing to remember is that we try and stay between the two planes; the bladder and the uterus. A fiber-by-fiber dissection makes the process easy. One layer goes to the bladder and the other slides over the cervix and vagina.
Visually we see the vascularity in each layer going with respective organs. This acts as a guardrail telling us where we might need to course correct.
There is a combination of medial and lateral approaches, which we use to eventually focus on the spot of endometriosis buildup.
Sometimes we will have to take a bold step in order to create a space for dissection. Doing so we take a part of the nodule towards the bladder and the other towards the uterus.
Key Surgical Step
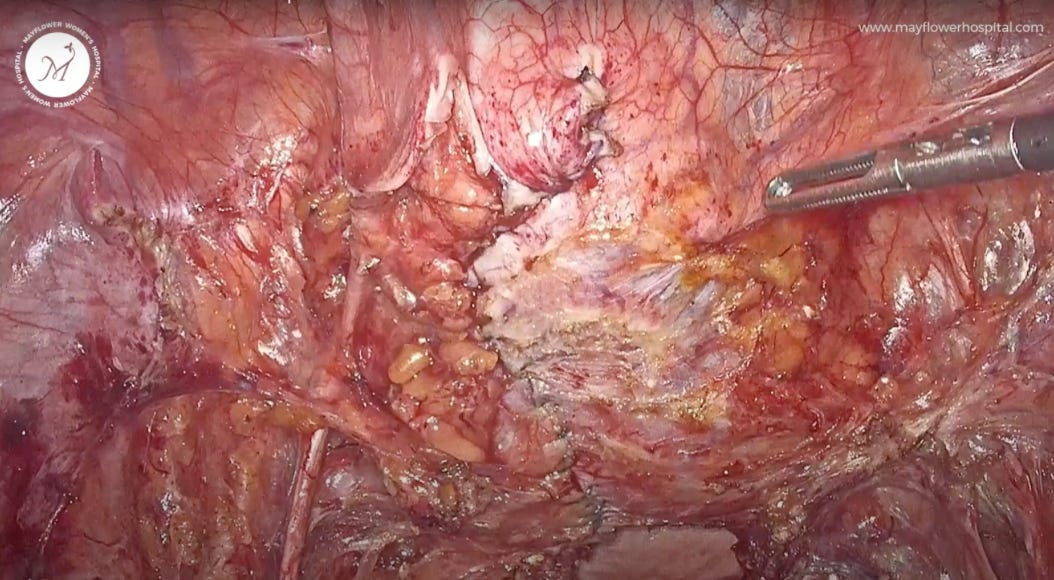
We open the bladder in the midline fashion and an Incision from the dome of the bladder to the nodule is placed.
In the process, we always make sure that there is no residual plaque left behind.
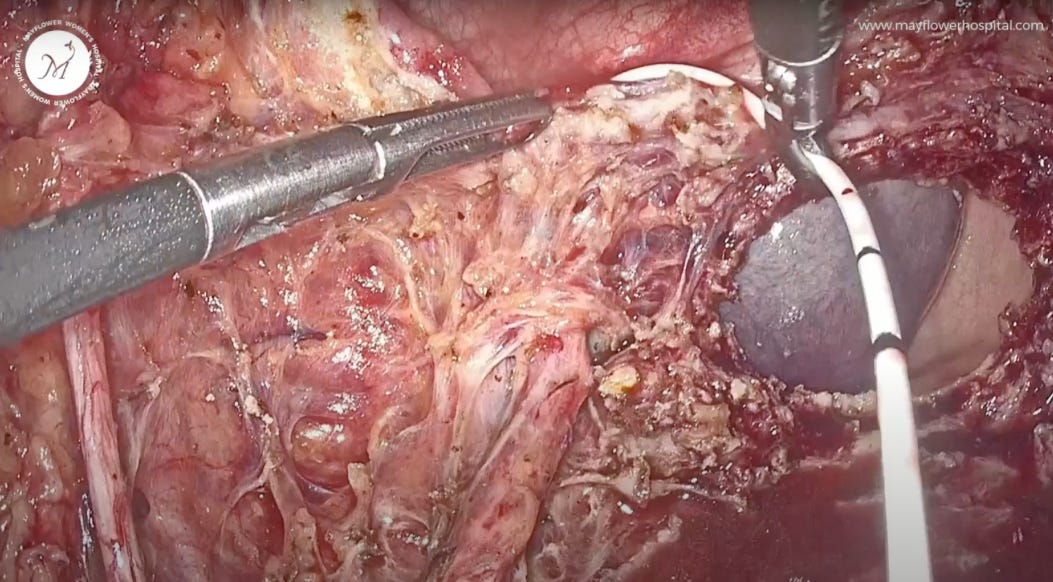
Cystoscopy told us that the ureter, its orifice and the trigone area are normal and hence we take extra care to not cause any damage to those areas. Once dissected from all sides, we excise the nodule.
Laparoscopic catheterisation is performed on the left side, with the ureteric orifice being in close proximity.
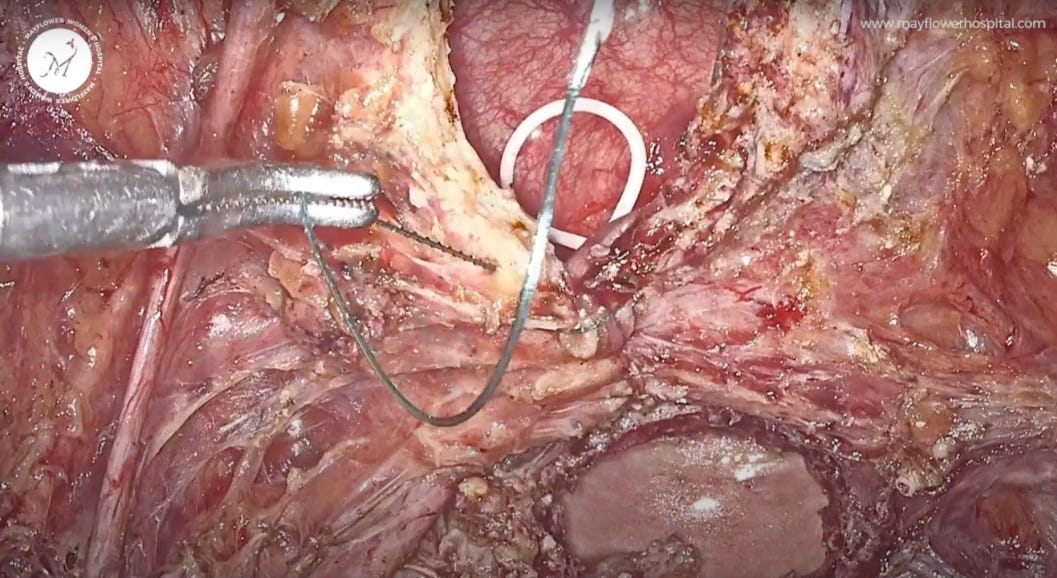
The bladder defect is sutured in a midline vertical continuous fashion. We take a 3-0 barbed suture and start from the lower end. Once an angle is secured, we start taking full-thickness bites and slowly move our way upwards.
Once done, we start from the upper end, secure an angle and in the same fashion we start suturing. Using this technique we secure both angles separately and there is uniform tension over the stitch line. This is essential in maintaining the structure of the bladder since it fills up and empties frequently.
One may choose to go for a second layer of seromuscular suturing or some reinforcement sutures if needed. But that’s a subjective call you as a surgeon must take in the moment. The aim here for suturing is to be tension-free and watertight.
Once we’ve confident, the bladder is filled, and we look for any leaks that might have occurred.
At the end, the vault is closed and an exit is made. On the 14th day, a cystogram is acquired, and the ureteric DJ stent and bladder catheter are removed.
While the theoretical aspects of this surgery are straightforward, it deals with complex and critical systems of the body that can make complications life-threatening, very quickly.
It’s important to counsel the patient, have a transparent risk-sharing prospectus and have a willingness to go above and beyond the call of duty.
Thanks for reading this far! Did you know that we also write a weekly Newsletter on the latest most interesting and worth-pondering aspects of gynaecology? The letter is called Pollen and you can use the button below to have a look and subscribe!
That’s it for this week! See you next time!










Amazing sir/madam. Thank you for sharing