Far up the Food Chain: Endo involvement around the Ileocecal Junction
A surgical walkthrough and tips to handle the involvement
The most common response we get when talking about GI tract involvement (especially places like the ileocecal junction) is that it’s rare. But that’s a misleading response. Sure, statistically, you can call it rare. But when you look at the numbers, you realise, it’s not that rare either.
Look at the existing literature around the presence of Endometriosis in women and you will find that a little over 1 in 10 women are carrying the disease and of those, anywhere between 3 to 37% have their gastro-intestinal systems involved.
That’s more common than finding someone wearing open toe shoes in summer on a street in Bangalore.
Meaning to say that if 5% of the world’s population has endometriosis, and about 2% might have their intestines involved, you’re looking at almost 14 crore vulva owners worldwide who at some time might display symptoms of endometriosis in the colon.
That’s a lot of people and that makes every location of the disease worth studying with intent and sincerity. And this also underscores the significant role that a GI surgeon plays in a surgery. At Mayflower, we’re lucky to have a team led by Dr. Lakshman Khiria equipped fully to deal with any eventuality we might face within the OR.
While the most common GI tract involvements are of the sigmoid colon and the rectum, they’re followed immediately by occurances at the ileum, appendix, and the cecum. source
Ileocecal involvement often might not have any symptoms till its too late. When it is symptomatic, the evidence might not directly point to endometriosis either. Cramps, vomiting, and acute intestinal obstruction are some symptoms when they do show up. source
No prizes of course for guessing that today’s edition is dedicated to the surgical steps involved in dealing with the ileocecal involvement of endometriosis.
Step 1: Mobilising the Appendix
Like we mobilise appendix in case of an appendectomy we mobilise the fat and parenchymal tissue around appendix.
Don't forget to perform some adhesiolysis if needed. Remember better the dissection and the better the adhesiolysis, clearner will be the excision margins and better the surgical outcome.
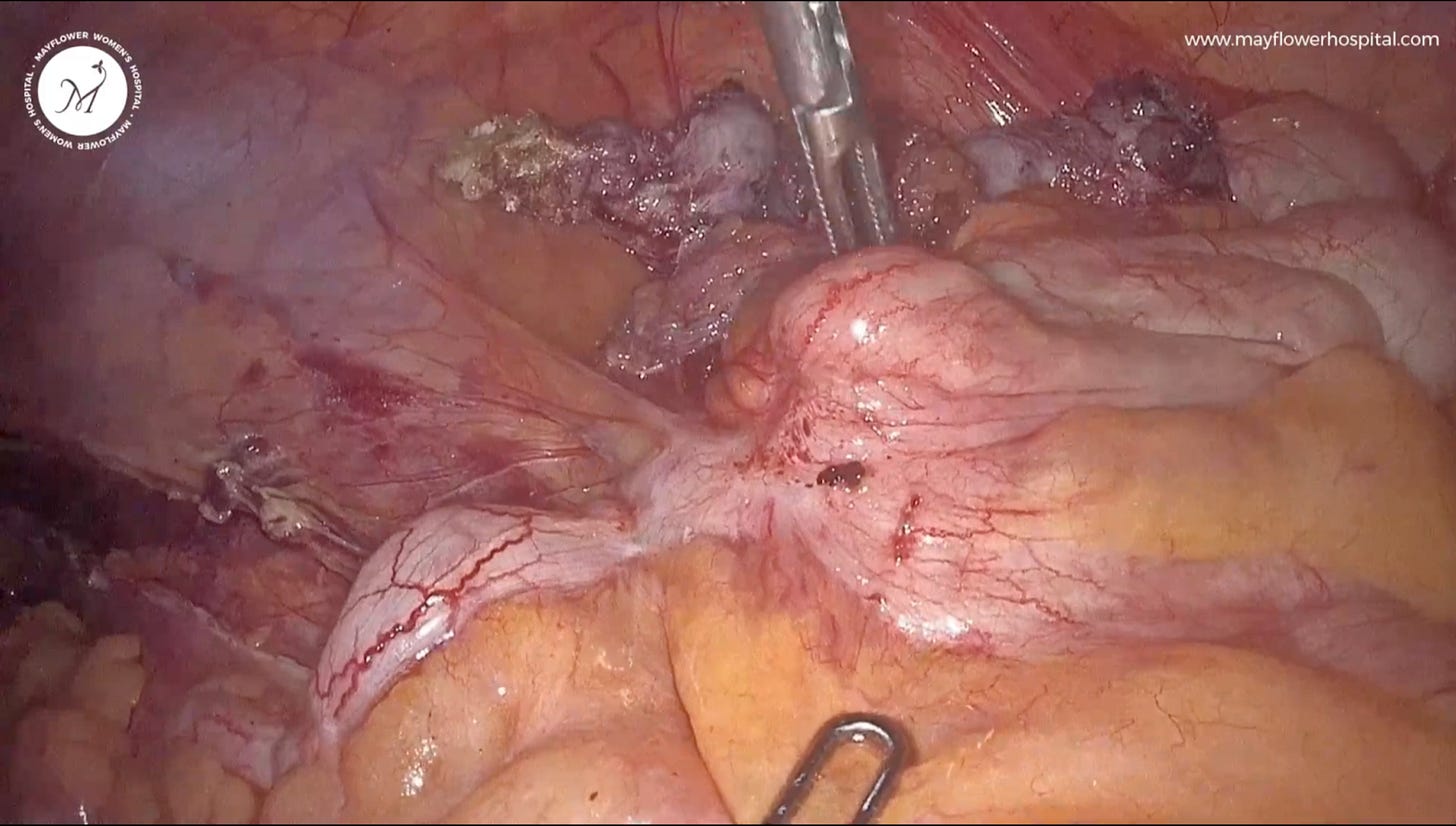
Step 2: Mobilisation of cecum and retroperitoneal dissection
To mobilise the cecum we dissect the parenchymal tissue surrounding it. A proper traction and counter traction is of paramount importance to protect the organ and surrounding structures from any undue damage owing to proximity or laxity of tissue. Small fiber by fiber dissection is prescribed making sure we don't injure the serosal surface of normal cecum.
What not to injure in an instance like this becomes important while ensuring a complete excision of the affected tissue.
As a pelvic surgeon we typically used to the vision of the pelvis, but here we are working in a different quadrant of abdomen and hence orientation is very important. Take ample time to orient yourself, keep the GI surgeon in close aide and advice, and then move ahead with the harmony.
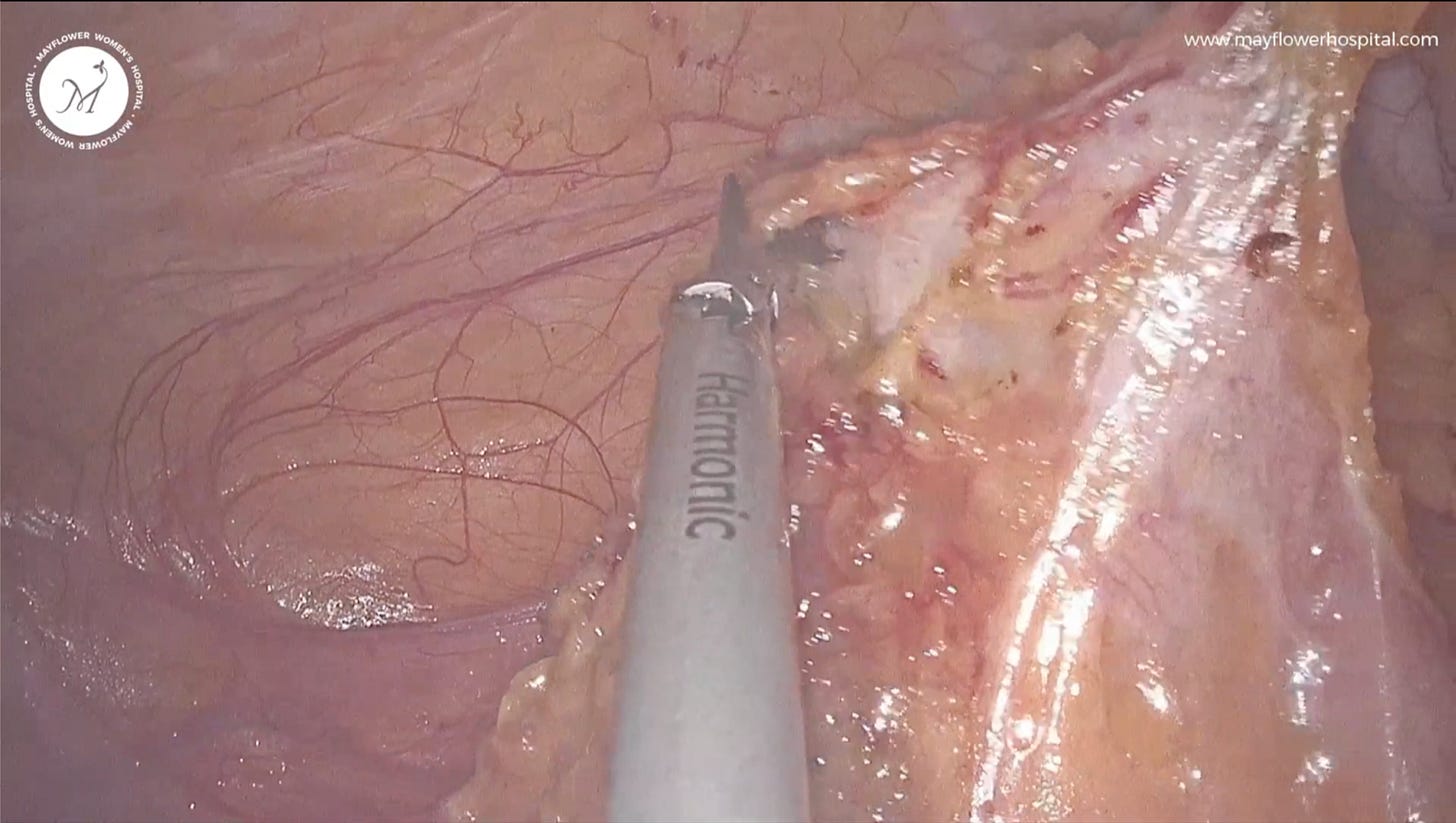
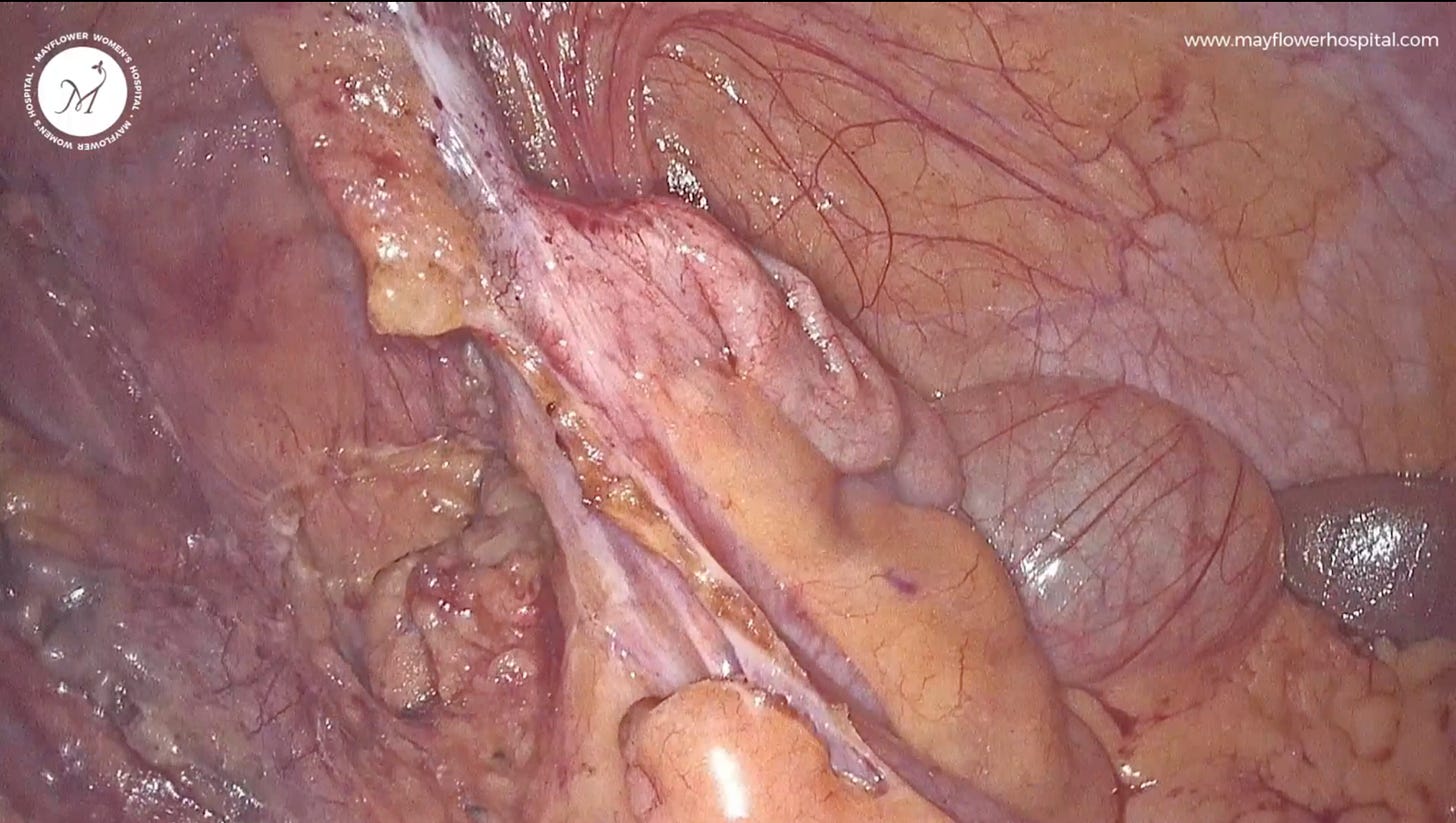
Step 3: Mobilisation of fat surrounding the endo nodule
This is a thumb rule of mobilisation: if fat exists, it belongs to the organ. So in any case we always mobilise the fat surrounding the pathology as opposed to mobilising the patology itself.
So we dissect along the margin of the fat surrounding the nodule’s anterior surface (less in this case), subsequently and more importantly, late move to the posterior aspect’s dissection in this case.
Fat also is a difficult candidate for dissection and can sometimes hide important anatomical structures behind it. That’s why we treat fat like a guide when it’s useful and, denude it when it isn’t
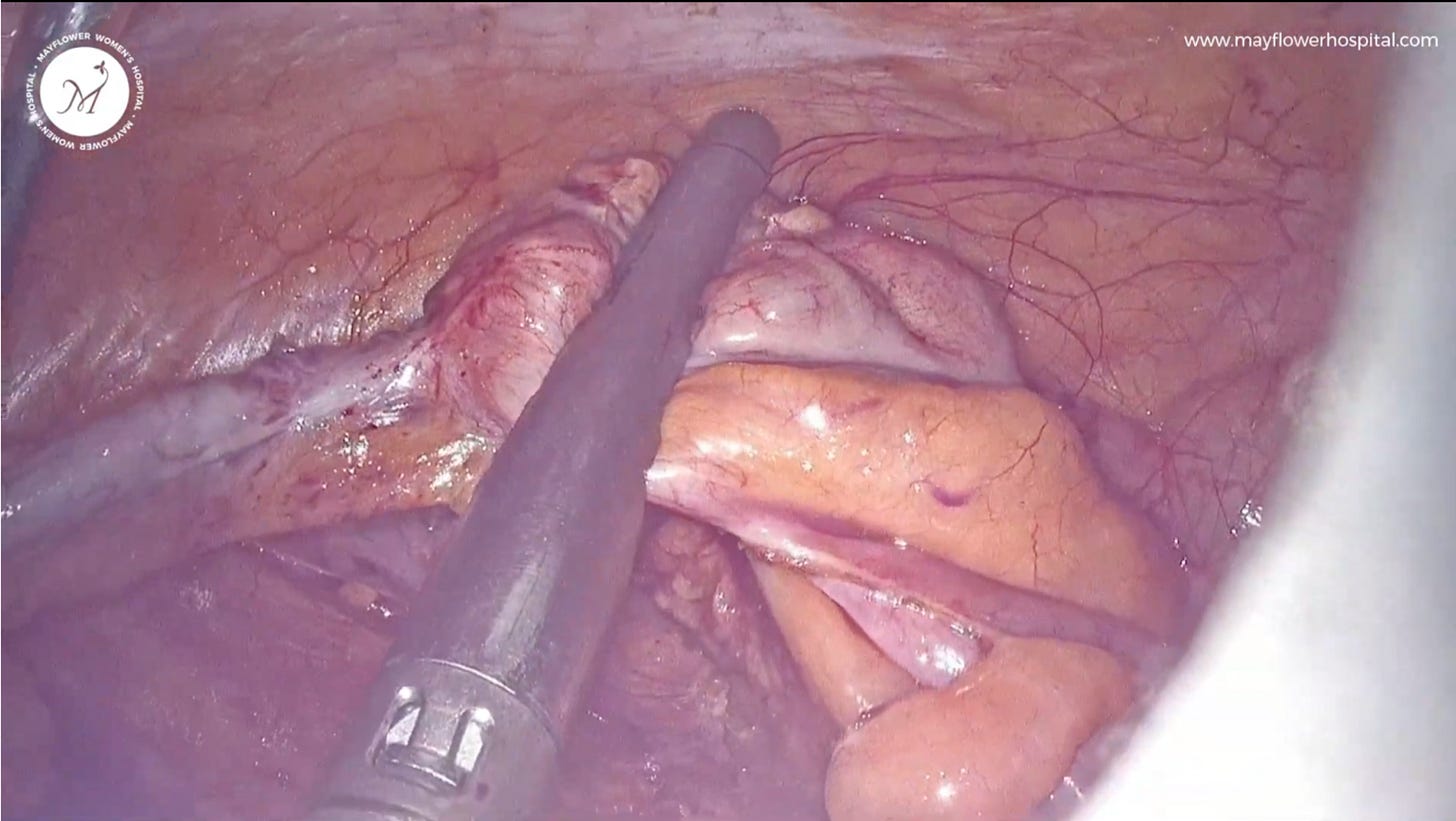
Step 4: Stapler Fire
We introduce the stapler, position the stapler and then fire it. Boom. There’s not much work there. No smarts needed. Infact, once you have the spot and the orientation, the less you think the better.
We will dedicate a complete session on stapplers here at EW in time to come. For now, an important point in this technique is that we make sure that the ileocecal junction itself is not involved.
Step 5: Reinforcement
Having difficulty in trusting systems isn’t always a bad thing. Especially when the system is new. To ensure the integrity of the stapler seal, we follow up with an additional layer of reinforcement of sero-muscularis layer over the stapler line.
It is done with polyglactin 910 (vicryl) 3-0 and in a continuous non locking fashion.
Once completed, homeostasis is checked and an exit is made.
With that our ileocecal management in endometriosis comes to a close. Of course each case we encounter is different and begs to be looked at as a separate case but these general steps will usually follow.