Anjali's Rare Bad Luck with Endometriosis
A story of adversity, perseverance, and relief in a case of uretric deep infiltrating endometriosis
Following is a true story. At the request of the patient, their name has been changed. Out of respect for the practice of surgery, the rest has been told exactly how it occurred.
Amongst the toughest cases of intrinsic involvement in endometriosis comes that of the involvement of the ureter. We covered dealing with ureteric involvement in detail in our edition on the 5 levels of ureteric dissection.
But we lied. There are more than 5 levels of dissection. 9 to be precise. These 4 new levels begin with the intrinsic involvement of the ureter. We left these out because they’re both rare and incredibly difficult to deal with. However, every once in a while we like to remind ourselves that when the disease goes hard, surgeons can go harder.
In today’s edition we go deep into a case of intrinsic involvement of the upper 2/3rd of the ureter in endometriosis, and how an end-to-end anastomosis can be performed to solve the problem.
Operated in late 2019, Anjali, a resident of Ahmedabad is the survivor we meet today. Mother to a toddler, Anjali had a generally difficult menstrual life with early onset pain. But like most women suffering from endometriosis, she wasn’t given the right diagnosis for a long period. It was only when the pain started to get chronic owing to peritoneal involvement, that she was referred to a higher center, operated twice, and eventually arrived at Mayflower.
Her past surgeries focused on cyst drainage, and hysterectomy, in the hope of alleviating pain in the short run. However, the active glandular nature of endometriosis can keep it going and growing well long after a TLH has been performed.
In this case, the disease thrived. Invading a good part of the ureters.
Ureteric involvements are always tricky. The disease has to really be aggressive to have any impact on the ureter to begin with. Why? The ureter is a mobile organ. It’s continuously moving and has a thin but flush web of mysentry around it. Endometriosis on the other hand needs time and peace to grow, something that ureter absolutely doesn’t provide.
This is also why we often see intense ureteric involvement coincide with anchoring adhesions around the ureter, and not just laminar growth around it.
Laminar growth however is still only an extrinsic involvement. It often gives way to an intrinsic involvement where the disease invades into the serosa of the ureter which first throttles the flow of urine and subsequently strictures the ureter completely. Hydronephrosis first, and renal failure later.
Coming in, Anjali’s symptoms were classic to patients of deep infiltrating endometriosis.
The symptoms were ruling her life
She was suffering from extreme mood swings
Frequently contracted urinary tract infections
Constantly felt as though none of the people around her understood her problem
Found it difficult to look after and care of her child
Was hesitant at engaging in intercourse because of a fear of pain
Was frustrated with doctors telling her it’s all in her head
She was showing signs of depression
And was fed up with multiple surgeries and no end in sight.
In all the glamor of tactful surgeries we often miss out on understanding why we do surgeries. “To remove disease” is the wrong answer. “To restore quality of life” is correct though.
After an extensive MRI, she was diagnosed with involvement in the right tubo-ovarian mass along with ureterohydro-nephrosis.
Surgical Plan
The plan was simple. The biggest task was to declutter the ureter and reconstruct it. Fortunately the involvement was in the upper 2/3rd segment and the kidney was still functioning well.
The right tubo-ovarian mass was densely adherent to the right parametrium, appendix, iliac vasculature, and the ureter. So the first step was to dissect and remove it.
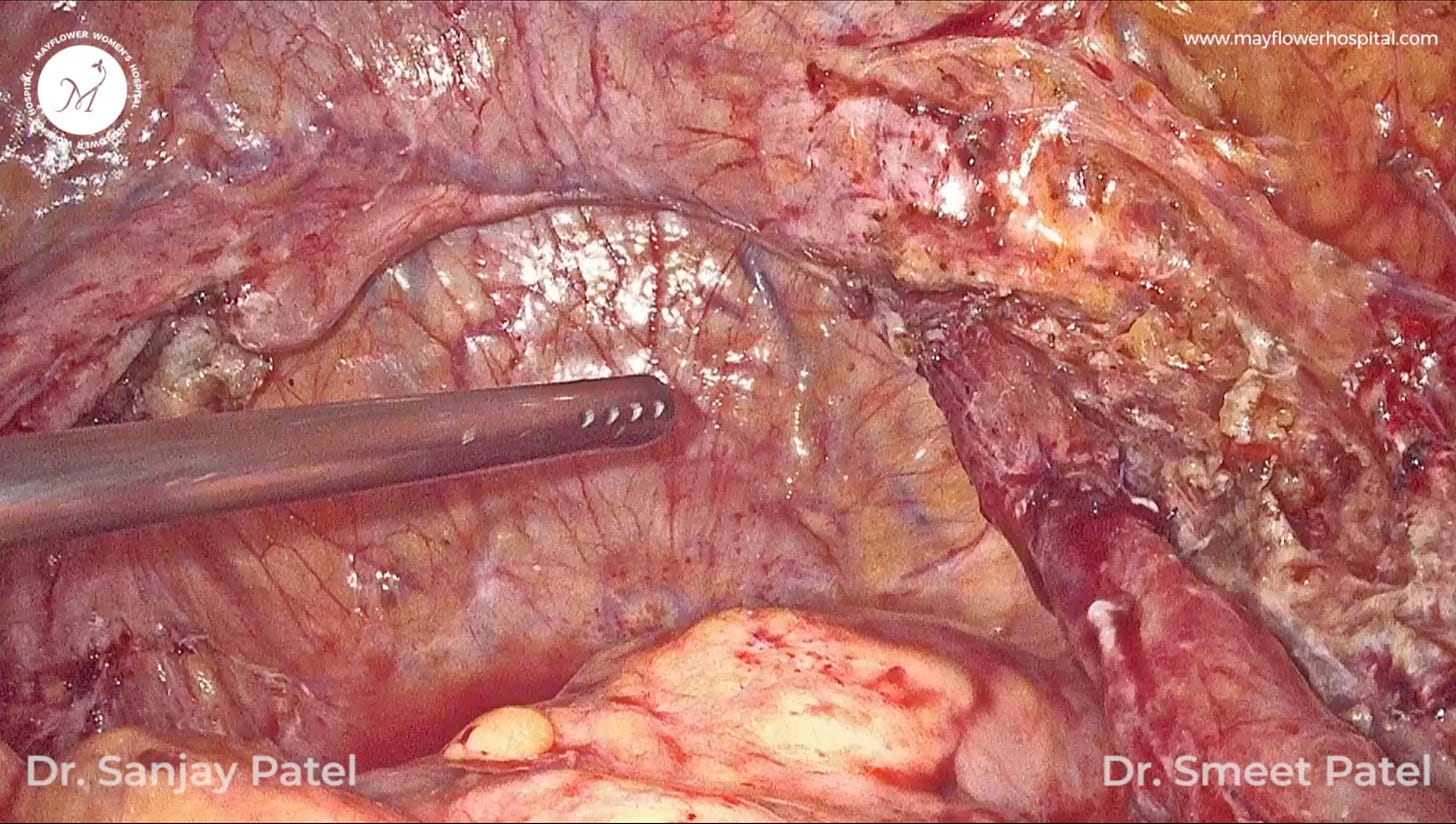
Now that we had the space, we began dissecting the ureter. For the most part, the disease will grow in layers, so our first step always remains the same, like unwrapping a birthday gift someone sent you. Find where the tape is, and begin opening from there.
Here, we go to the brim of the pelvis, place a knick, and start dissecting anteriorly while giving traction transversely.
Side-note: there is no traction without counter traction. And the plane of traction gets decided by the line that connects the two graspers giving the traction. So it’s very important that you pick the right place as perpendicular to the line of dissection as possible.
In case of hydro-uretero-nephrosis the ureter is enlarged upstream from the point of obstruction and owing to the expansion, the walls become thinner. This puts the ureter at a greater risk of being injured via an energy source so being extra careful is very important.
Side-note: tease laterally, cut vertically. Only use the tip of the harmonic scalpel. Dissect fiber by fiber.
The virgin gateway approach (as explained in this older issue) is taken for uretric dissection. The organ is dissected 360 degrees while preserving the mysentry. This is the most important aspect of conducting this procedure as the mysentry plays an important role in the functioning, and post op recovery of the ureter.
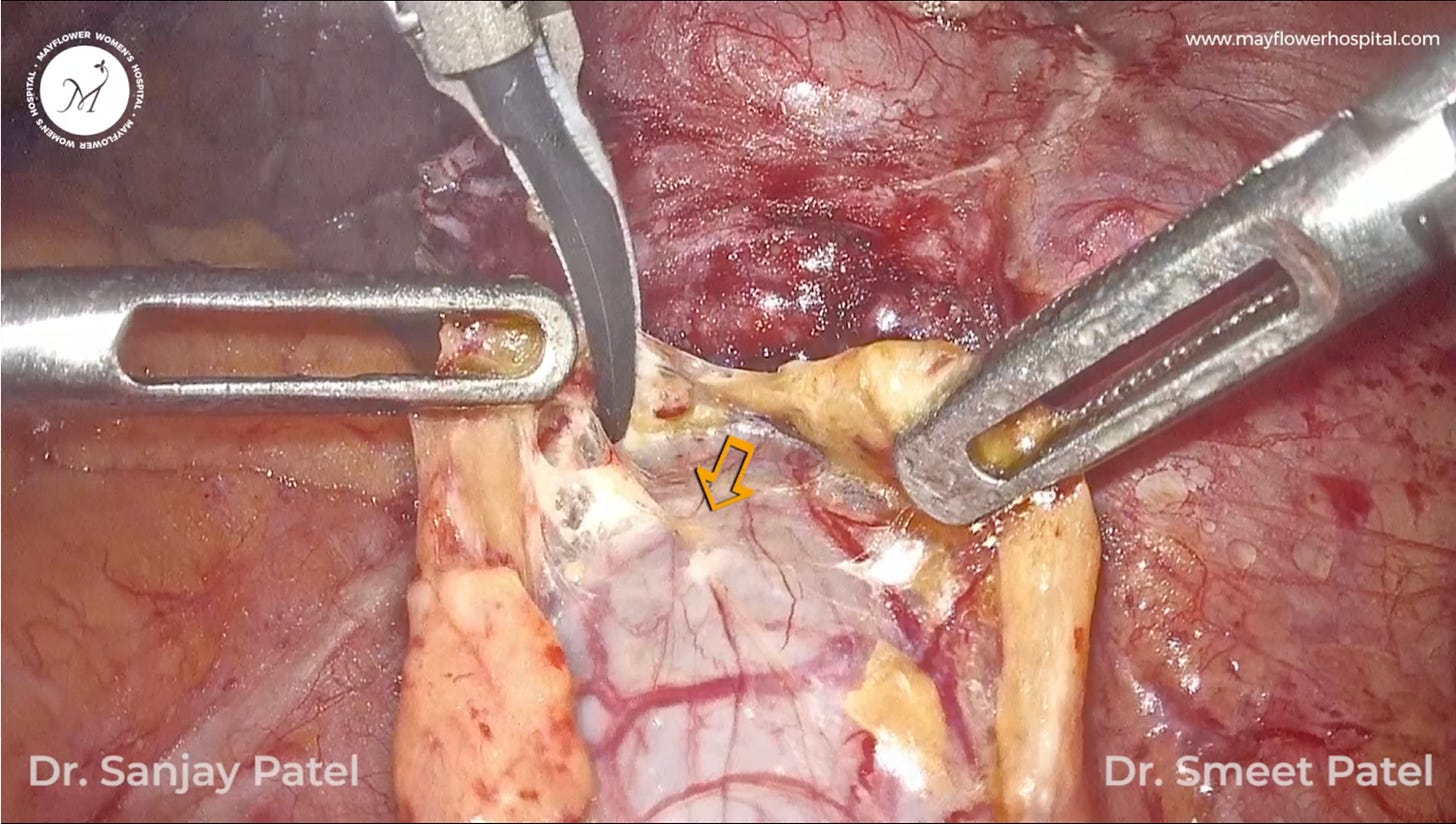
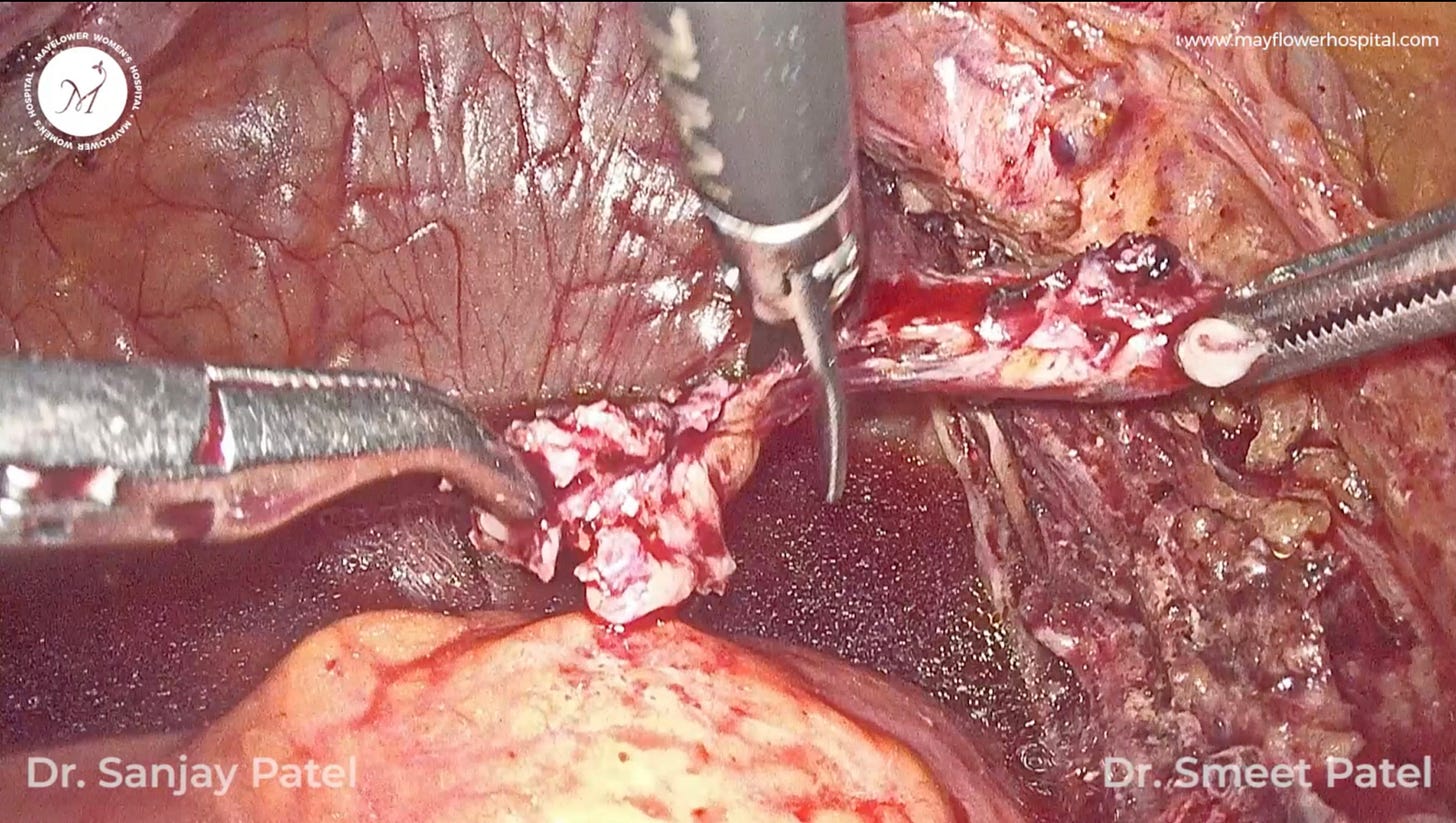
The point of intrinsic involvement is identified and the proximal part is dissected off with cold scissors.
While the distal end is freed from the involved endometriosis plaque
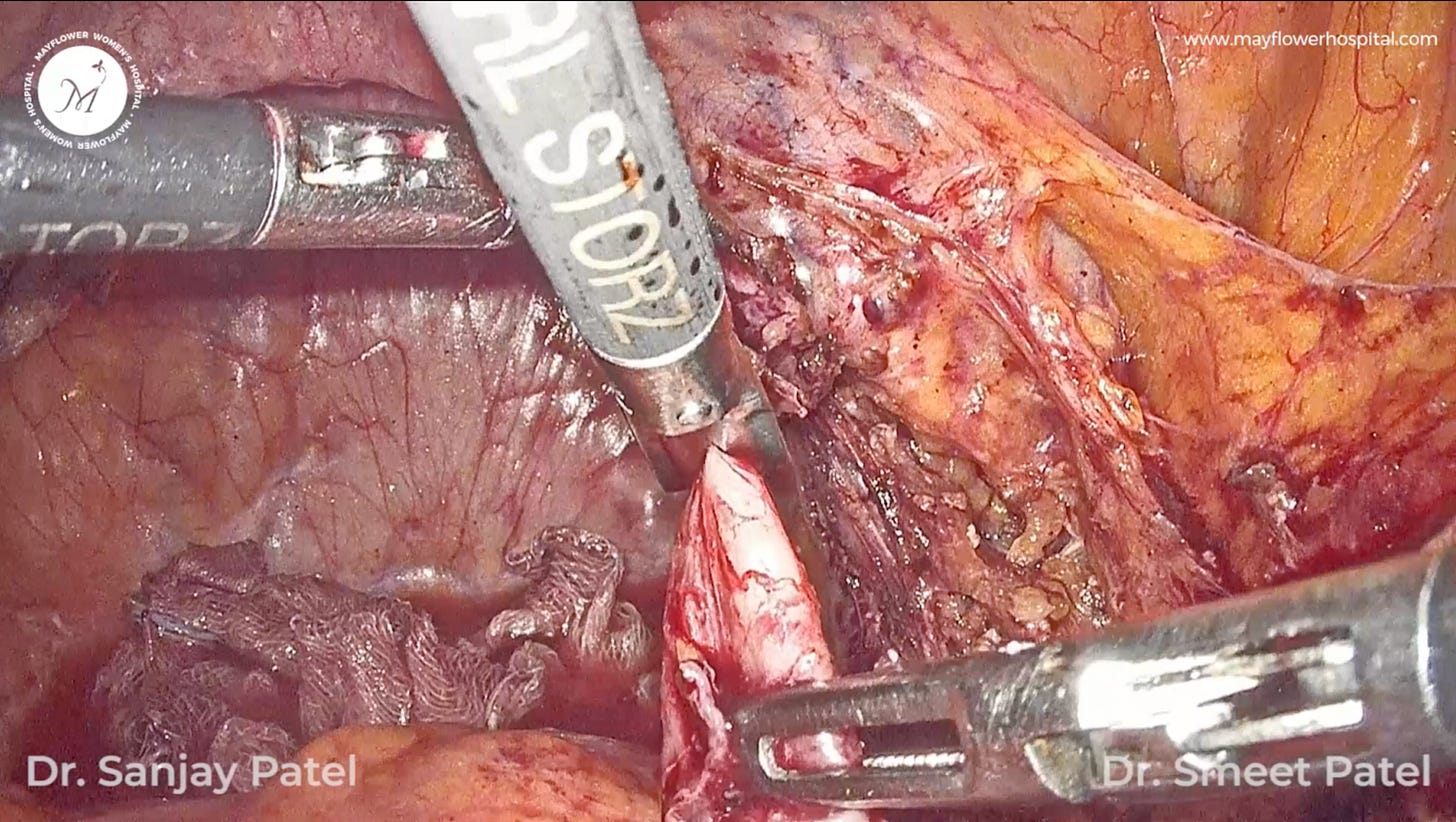
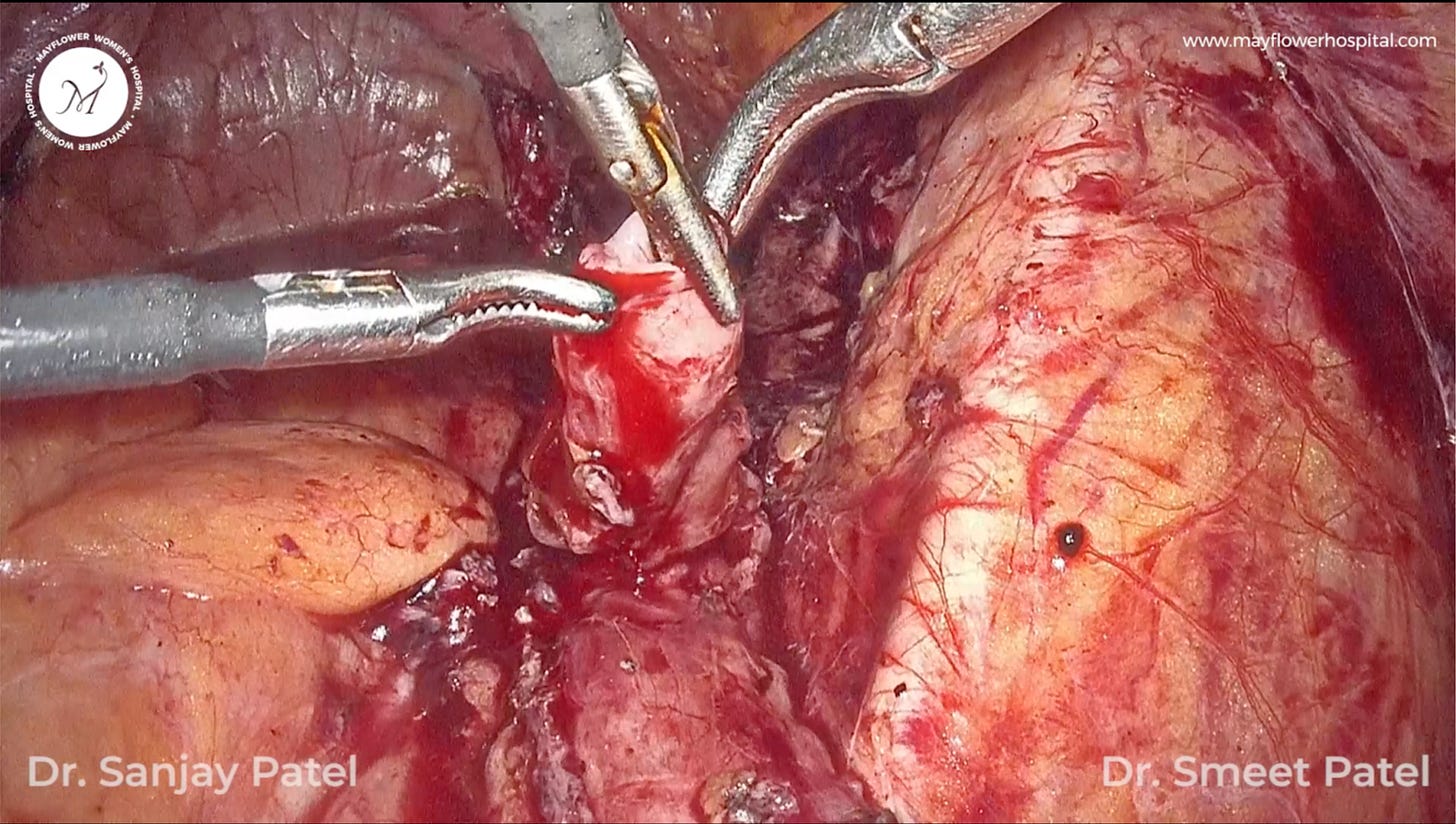
Having removed the disease infested part, we now have two freshly dissected clean cut ends of the ureter, brand new. Both the ends are spatulated at the margins and a laparoscopic stenting is done.
Now comes the climax. One inadvertent outcome of the end-to-end suturing process of the ureter could be suture induced torsion from the pulling of the purse string sutures. To avoid that from happening, we first approximate the ureter end to end with minimum twisting and then place a 12 o clock suture on the distal end and tie it to the sides. This will act as a guide to maintain the axis of the ureter through the process.
At Least 6 purse string sutures are taken 360 degrees around the ureter. All the sutures are taken in an interrupted fashion through the full thickness of the ureter to ensure a proper seal at the junction.
And that’s it. Looks simple right? It is. If you keep all the first principles in mind, and act with a good intention, it’s not really that hard.
Anjali saw a health recovery post op and was discharged on day 4. Her DJ stent was removed after 4 weeks, a CT urogram was performed with IV contrast and reported normal findings, followed by consultations at 3, 6, and 12 months.
She now only visits Mayflower to enjoy the world famous bhel served at cafe Mito, and the occasional chai that she shares with us on her visits.
Over the months we have observed
A consistent improvement in pain scores
A considerable improvement in genitourinary tract symptoms
A renewed quality of life and will to thrive
She feels confident and interacts frequently with friends and family
Has a satisfactory sex life
And is able to take ample time out for her child’s early days at school
These encounters often help us gather perspective on why we do what we do. The purpose of surgery is a better quality of life. The labor of end to end suturing is meaningless, and frivolous if it doesn’t result in the outcome that we observed. Had this been possible through an easier route, I would’ve been the first person to pick it. Had there been a GnRH agonist that could make her pain go away, I would’ve prescribed it in a beat. But it simply doesn’t work.
As I write this edition of Endometriosis Weekly, a good, total, restorative, and holistic surgery in the first go is the most effective and easy solution to endometriosis.