The Road to Denonivillar's Fascia
In surgery, like in life, somtimes it's about the journey and not the destination
“ What’s on the other side of the denoniviller’s fascia?” a slightly confused fellow once asked me hesitatingly inside the OT. “Nothing” I said, “it’s open air, it’s one end of the pelvic cavity, right?”
“oh…” she said slightly puzzled, “why are we going there then?”
“Because along the way we will find something incredible. Sometimes, it’s about the destination, it’s about the journey.”
Before we have any conversation about the denoniviller’s fascia, what it is, where it’s located, and how we get there, it’s important that we have a word about spaces.
Most spaces that we discuss in surgery are all real spaces. They exist, and we use them as room to perform surgery. But every once in a while, they are not enough. You must go in and create a space. Laparoscopy allows us the benefit to alter spaces to suit our needs. Spaces that help us:
Enhance our surgeries
Give better outcome
Proper visualization
Helps in demarcation of diseases/pathology
Completer removal of disease
Plan further steps of surgeries
One such space is Denoniviller’s.
In the pelvis we need to demarcate this in many of our surgeries ranging from endometriosis, and radical hysterectomy, all the way to vaginal, and cervical pathology surgeries.
The Surgical Approach
The road to denonvilliers starts at the pelvic brim
We take the road both ways (from right as well as from left); beginning with a dissection of the medial para rectal space, opening it further towards the caudal part where between the rectum and vagina merger, the three walls (vaginal, rectal, pelvic) meet to form the denonvillers space.
On the right side of the patient : we as surgeons hold the mesocolonic fat at the pelvic brim and apply traction. On the other side the assistant surgeon holds the parenchymal tissue just medial to the ureter and counter traction is applied.
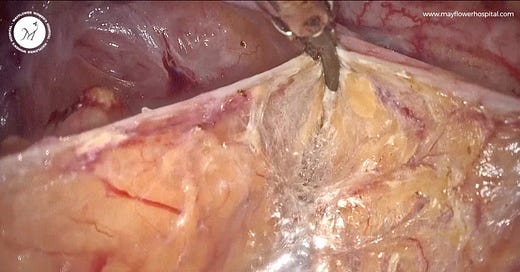
Beneath the peritoneum another potential space exists called the MPS or the medial pararectal space. A knick is placed and we see a beautiful cavitational effect. We follow this cavitational effect and trace it caudally. While dissecting the MPS we make sure to preserve the hypogastric nerve.
A similar procedure is performed on the left hand side as well.
<Traction> parenchymal tissue just medial to the ureter
<Counter traction> mesocolonic fat at the pelvic brim
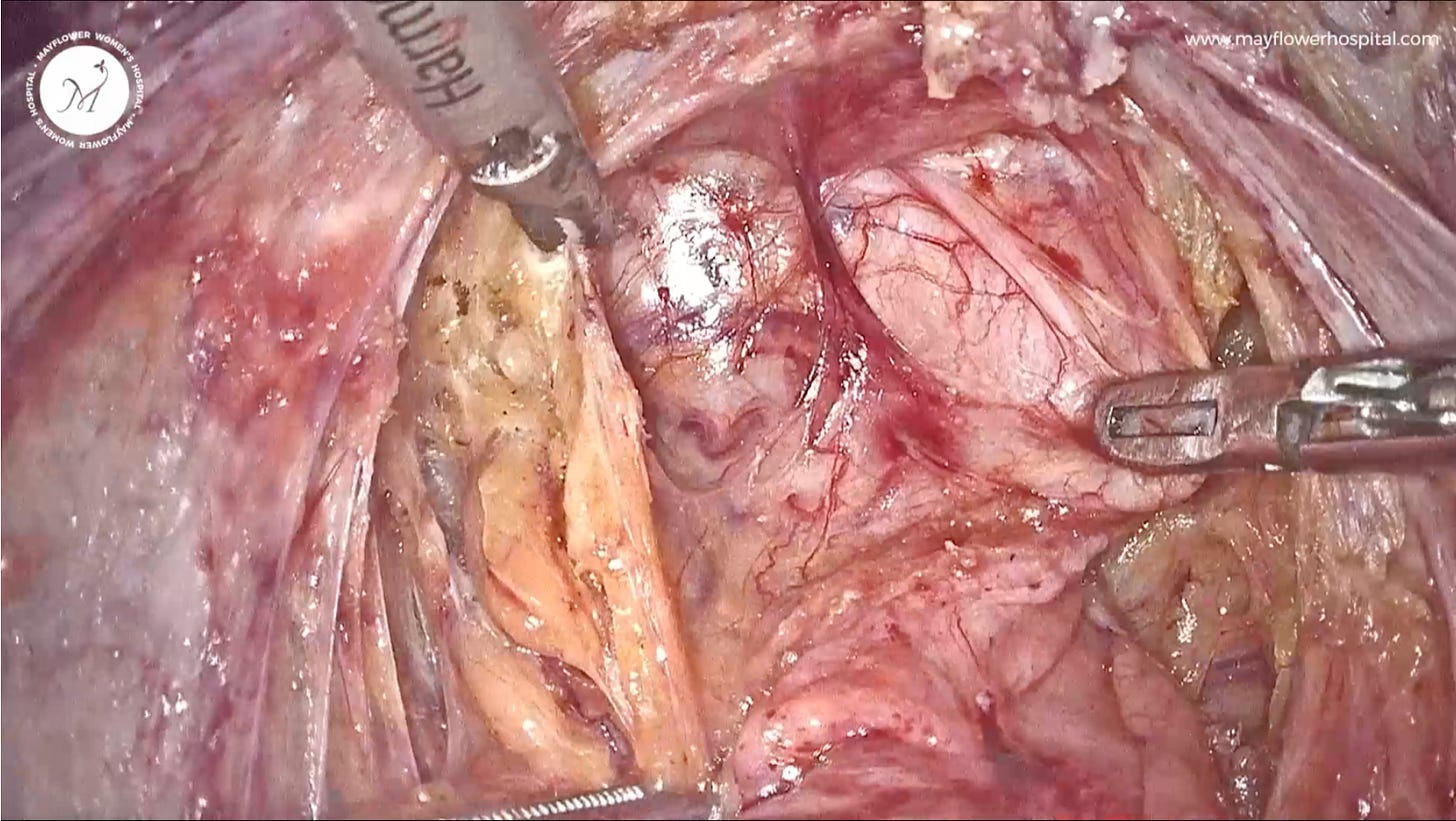
As we maintain traction (MPS) on both the sides and the space opens up we will notice that towards the caudal region the two MPS spaces will merge to form the Denonvilliers space.
As we dissect further in the caudal region; it’s important to follow a thumb rule that one layer of the peritoneum goes towards the vagina, and the other layer goes towards the rectum.
We can clearly see the mesenchymal vascularity going with rectum and vagina respectively
Pro dissection tip: Always dissect in a way that the fat stays with the rectum
Now that we see the entire rectum, we can:
Easilly remove recto-cervicalpathologies
Map endo nodules
Dissect rectal endo nodueles
Approach mayflower butterfly peritonectomy
And much more…
As an artist - we always focus on the dissection - a neat and clean dissection always gives us pleasure and its this pleasure that keeps bringing us back to surgery.
That’s it for this week. See you in the next one!