The Mathematics of Endometriosis Surgery - Ep 4 - Peritonectomy
Ever packed too much for a holiday? I do it all the time. It’s mostly fueled by this internal dialogue of what ifs. What if I run into the prince of Abu Dhabi and he wants to invite me for dinner? Better pack a tuxedo. What if we’ve partied too hard and then have to go to an after party but we’re still in beach clothes? Better pack an extra pair.
Before I know it I am 7kgs overweight and then have to start the painful process of shedding. When all is done and I show up to the hotel of my destination with a bag bursting at its seams, I will still struggle finding that one pair of socks that go well with an outfit. I remember packing them but they’re nowhere to be found in this hot mess.
At that moment, deep in my heart I know I am only going to find that pair once I’m back home. And I will find it nowhere else but in some corner of this bag.
“But guys! why are we talking about vacation packing today? I have a surgery to do! Get to the point!”
Yes yes yes. You see the pelvis is a lot like an overpacked bag (seriously? so much buildup for this one metaphor?) and a lot of our job is like trying to find that pair of socks tucked away somewhere in the bag.
But unlike a bag, we can’t really unpack the human body. In fact, we wish to move as few things around as possible, and find the sock, and remove it without really moving any other piece of clothing. We can shift things around but we can’t take anything out.
Obviously, we’re going to need more space, all of which was lost when we packed the bag to its brim. Thankfully, there are some ways to solve this.
We can create a space
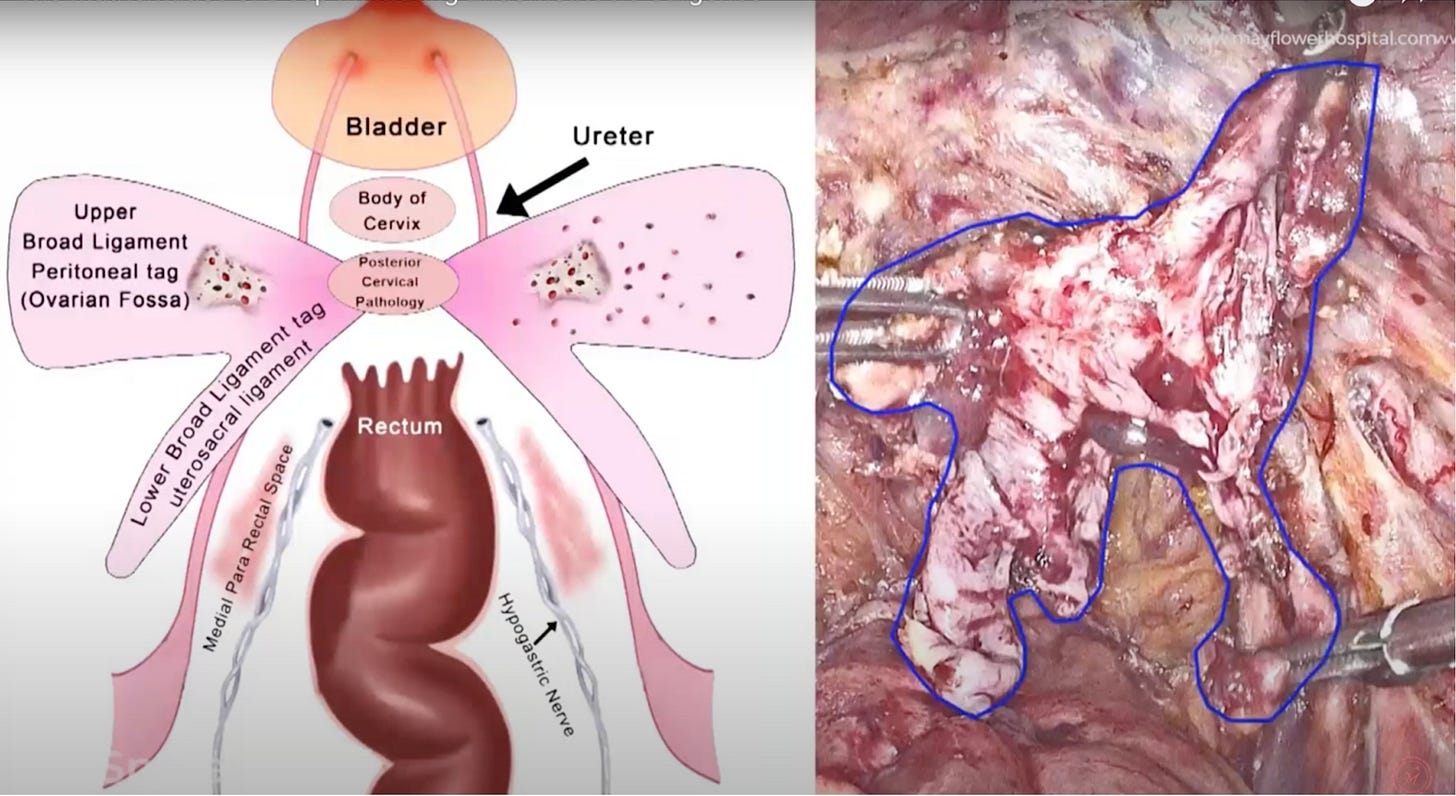
Using CO2 injection to inflate the pelvis is just one way of creating tool and operating space. But even then, the organs are often adherent with one another especially in cases of deep infiltrating endometriosis. That’s when we find the need to go in and create spaces. The Medial Pararectal Space or MPS is one such created space.
In the diagram below taken from this Springer article you can see the pararectal space in the peritoneal fold.
Para-rectal refers to the area around the periphery of the rectum on the two sides. Medial because it is towards the centre and not the outside.
This is a created space because it doesn’t exist as an empty space or a designated region but instead is found through a careful dissection of the peritoneum.
Through this dissection, we are able to access parts of the pelvis in a very congested multi organ zone that is also ergonomically difficult to reach.
This is critical also because owing to its rich vasculature and pervasive connectivity, the peritoneum acts as a highway for endometriosis, spreading from one point to the other, taking the disease to several places. Which is why sometimes we dissect the entire peritoneum en-bloc. Which is called the butterfly peritonectomy.
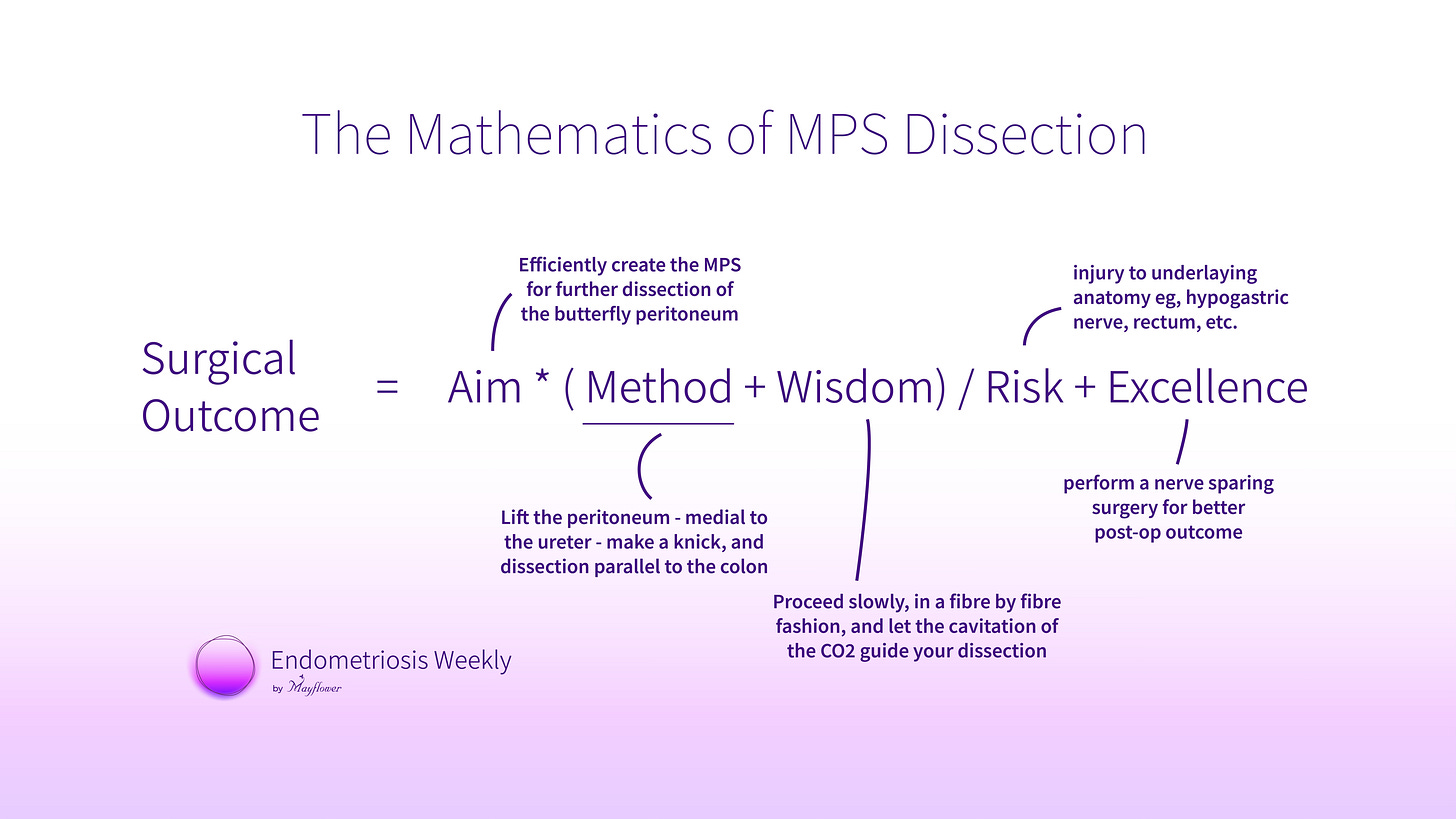
It is a step at start’s at the bottom and that’s exactly why we are first talking about the medial para-rectal space dissection on the peritoneum today. The aim is simple, create the space without creating any other problems.
One of the biggest risks here is nerve injury and in particular an injury to the hypogastric nerve (hGN) and its branches. An injury to the hGN can result in increased bladder tone, and dyspareunia among other problems, leading to weeks of post recovery time. Preserving this nerve is essential in performing this step.
Surgical excellence here lies in carefully dissecting the peritoneum so as to perform a nerve sparing surgery. It demands the patience of fibre by fiber dissection as you move forward. Any amount of hurry or negligence, and we will face weeks of post-op recovery and distress.
The figure below illustrates the presence of the hypogastric nerve in the process of dissecting the peritoneum.
At this point we have performed bilateral uretrolysis, followed by a bialateral MPS dissection keeping all the major vasculature, ureter, HGN and colon separate. What is left is the tissue mass with nodules that can now be easily removed.
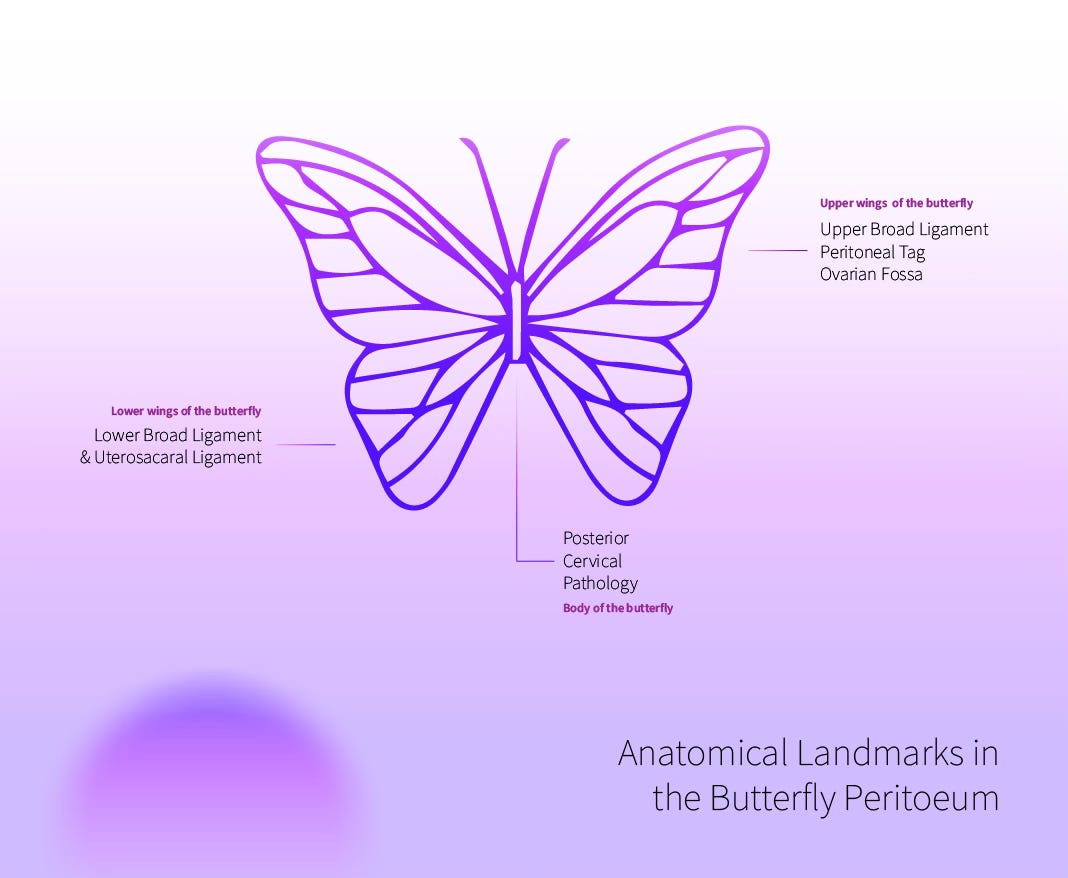
This is when we make way for the next step. The Mayflower Butterfly Peritonectomy. It involves the complete and en-bloc dissection of the entire peritoneum of the butterfly. Because the team at mayflower led by Dr. Sanjay Patel was the first to describe an efficient method of performing this procedure, it was named after the hospital.
A detailed walk through of the Mayflower Butterfly Peritonectomy is available on our YouTube channel and was also described in one of our older editions.
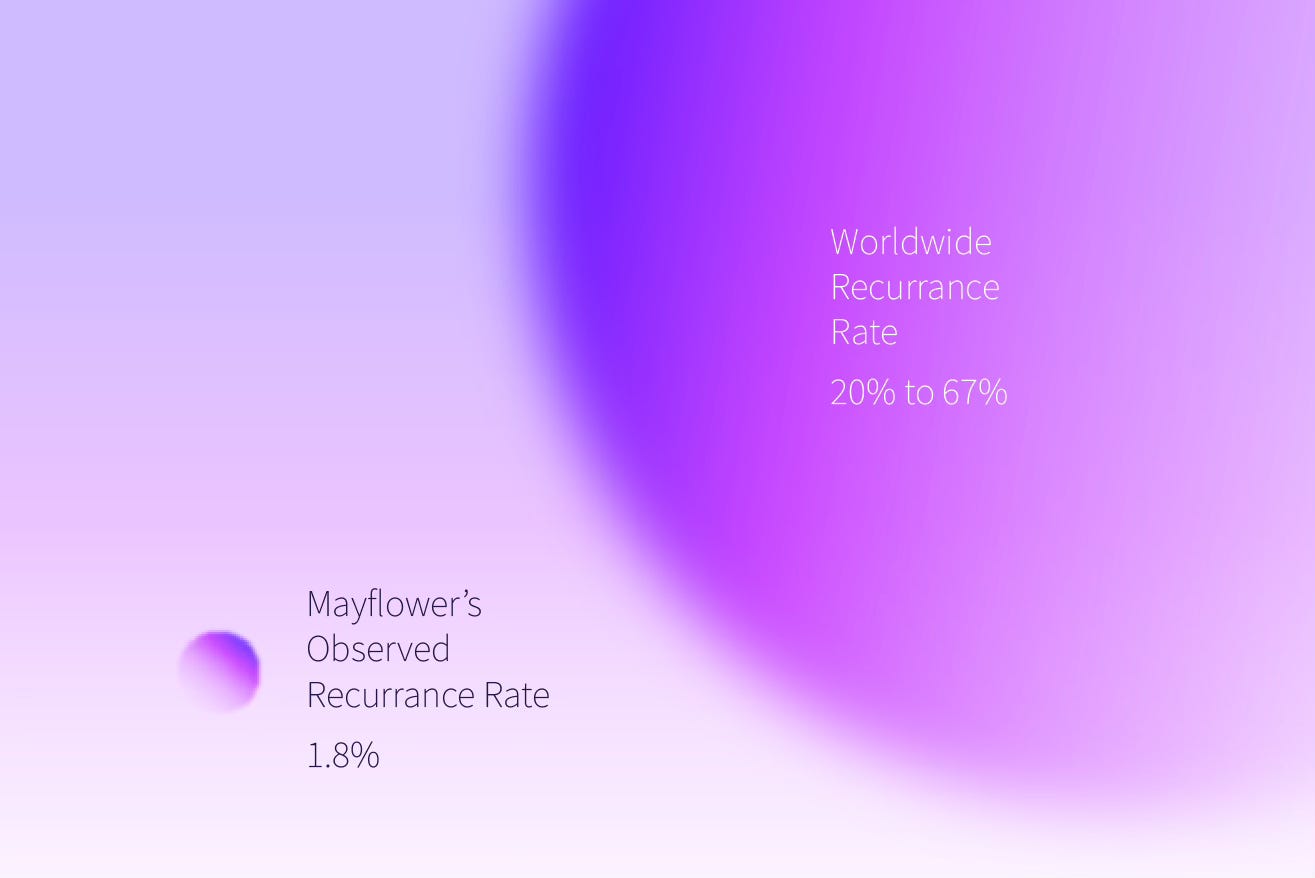
This procedure is also of landmark importance because it helped us reach a sub 2% observed recurrence rate while all other benchmarks showed a recurrence rate significantly higher, depending on who you asked. Leftover nodules on the peritoneum were culprits in cases of DIE and it is possible today to hypothesise that they are the reason recurrance remains high.
MPS dissection has helped us achieve two key objectives. The bigger is space creation. It has given us enough room to further our surgery. And secondly we’ve identified and secured all critical organs ensuring minimum collateral damage.
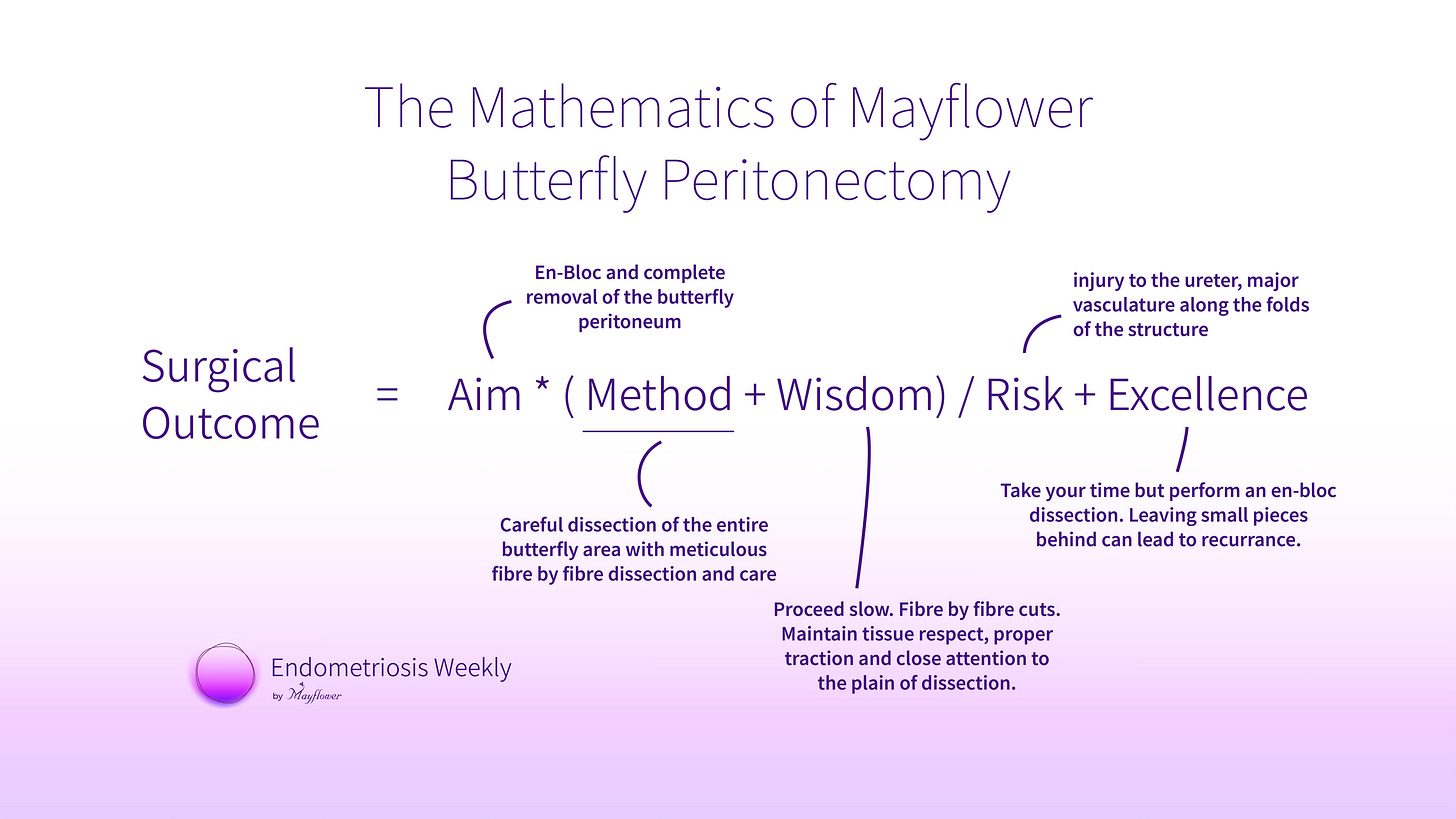
Moving on to Butterfly Peritonectomy, let’s get to the mathematics of it first.
The whole affected peritoneum of the uterosacral ligament, affected peritoneum of the posterior broad ligament, and posterior cervical pathology is removed en bloc.
A varying surgical school of thought is to go piece meal, sometimes when it is difficult to perform the procedure en bloc and other times when conventional wisdom suggests we only remove nodules. However, years of work here at mayflower has helped us understand that this region is laden with active endometriotic nodules and even the best of surgical procedures sometimes leaves behind large chances of recurrence. We’ve therefore taken the wisdom of an en bloc removal and turned it into our standard procedure with cases of DIE, especially when we are attempting fertility preservation.
Here’s an easy illustration from our previous article, helping you understand the anatomy and analogy better.
Once you’ve performed this step, all you really need to do next is perform the harder but more obvious and visually confirmed procedures that will further help restore a disease free anatomy, reduce symptoms, and eventually give the patient a pain free life.
This procedure has helped us with an observed recurrence rate of less than 2% and we have a strong conviction that inputs and innovations by surgeons from across the globe will only make it better.
And that’s it from us this week. We will be back next week with something more exciting.
Peace! ✌🏻