The Mathematics of Endometriosis Surgery - Ep 1
A 4 part series where we delve into excellence driving actions in specific procedures for DIE
Breaking things down to their first principles and solving them is our favourite hobby. First Principles, simply speaking are the fundamental operative principles behind anything complex that we see around us.
Take the stock market for example. You might think that things like candlestick charts and alpha or beta values, or some other breakout patterns are what’s at play. But really, what truly moves the stock market is a simple equation of supply and demand. If there are people willing to sell at a price slightly lower than the maximum price anyone is willing to pay, the market moves down. If someone is willing to pay just a little more for something than the highest of what a seller is asking, the market moves up.
That’s it. Everything else affects this basic principle. Nothing is more important than this. It’s the first principle of the stock market. The most fundamental, unresolvable attribute of a system.
In today’s edition, we take that first principles approach to surgery in deep infiltrating endometriosis (DIE) and break down how we can achieve a level of excellence in performing a procedure. Any procedure.
We have written this across 4 different editions to begin with and will add more as time goes by.
Today’s edition deals with Colon Mobilisation.
So let’s get started.
Before we get to colon mobilisation, let’s first address the elephant in the room.
What does mathematics have to do with surgery? Why are we complicating something that’s already complicated?
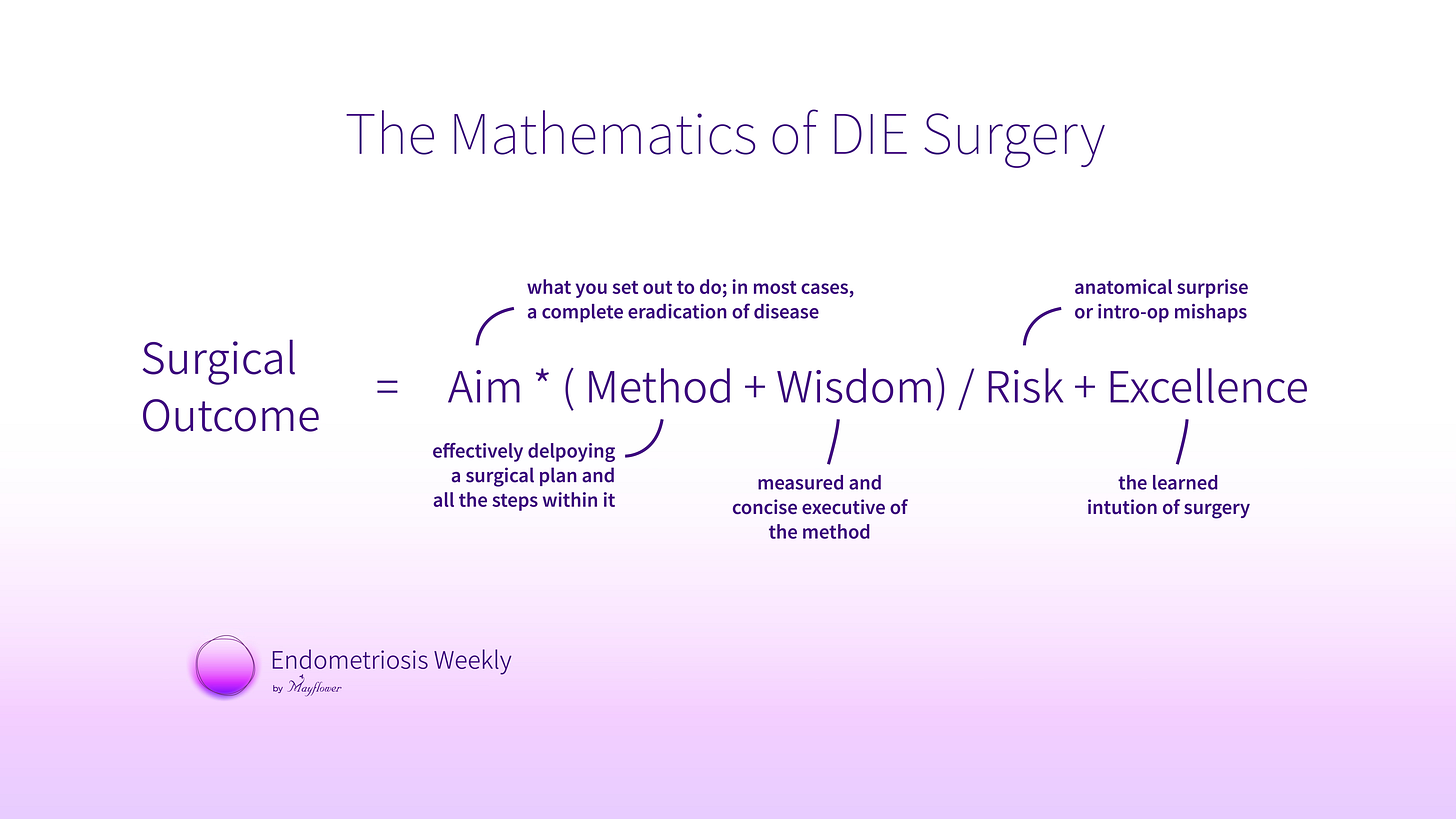
When thinking about the first principles of surgery and the various steps involved in a typical DIE surgery, understood that there was some relationship between the various aspects of any give procedure.
Let’s first list what makes for a good procedure
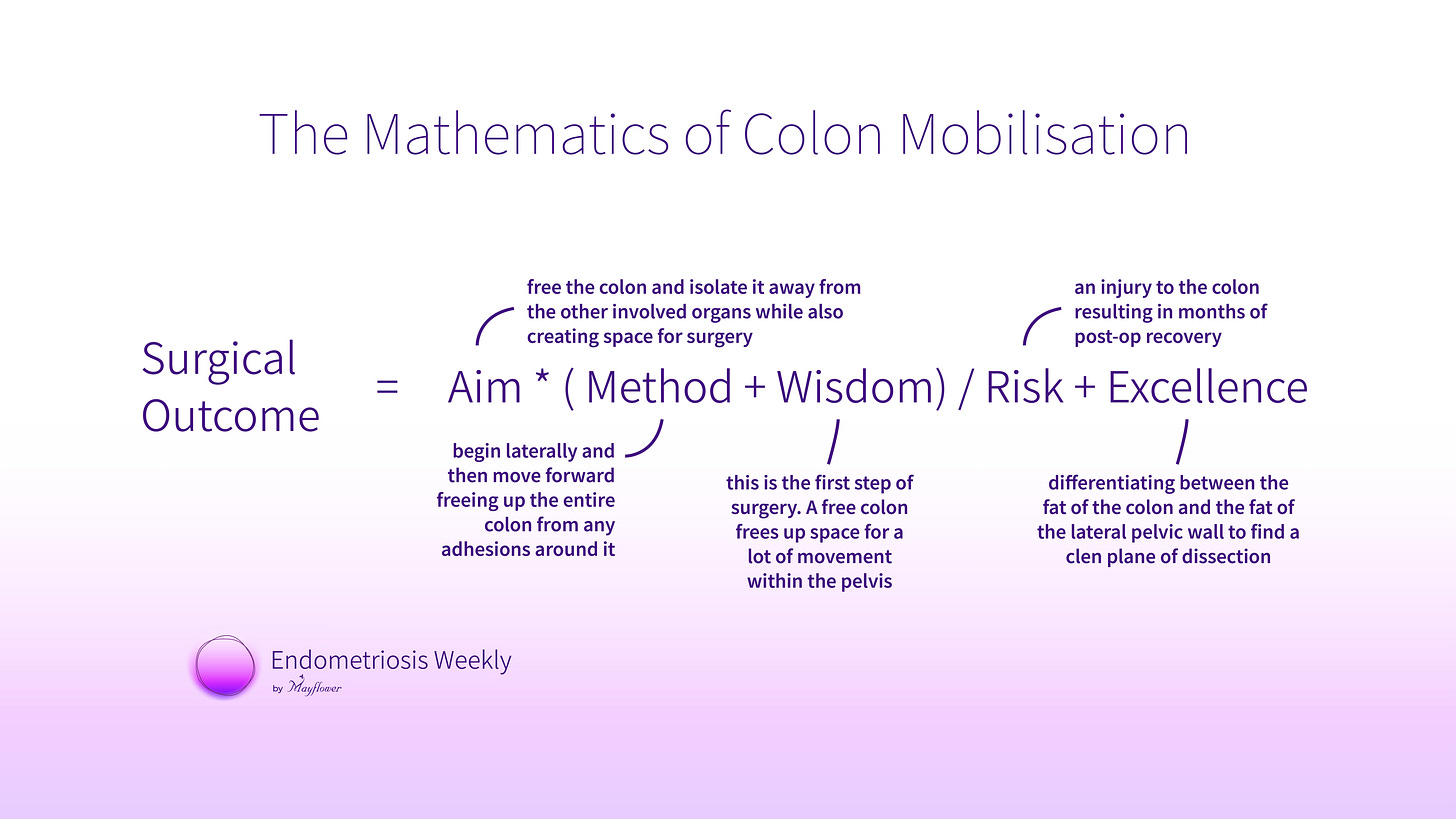
Aim - there’s something you want to achieve with a procedure. It could be space creation, nodule dissection, anastomosis, anything. But you have an aim. Always.
Method - there is a predetermined method to achieving that aim. This method gets refined over time but there always is a prescribed way of getting to your aim.
Wisdom - Over time as you work with the method again and again you realise that some things didn’t really come with the prescription manual or the method. This is the tacit knowledge of every surgeon.
Risk - with every method there is an inherent risk, a value you want to minimise as much as possible. Uncertainty is a reality of life but a poison for a healthcare business.
Excellence - if you do something for long enough, you evolve a combination of judgements and practices that help you build excellence. That becomes the reason people call you to conferences and want to watch you perform a surgery live.
These factors interact with one another to build what we call the mathematical function of surgical outcome. It’s a bit of a gimmick but it’s a great framework to start thinking about procedures.
At the risk of sounding arrogant, we’ve put it down quite neatly if you ask me. It’s simple. The method and your wisdom of using the method form the core of what brings about the outcome in any procedure.
When you aim is clear, and accurate, the outcome gets multiple by that clarity just as much. Poor clarity and the execution of a method that has conflicting aims can wreck havoc on the lives of patients.
Unfortunately, sometimes the aim of a surgery is to make marginal profits. Poor preparation, arrogance, under-diagnosis, and several other reasons could lead a surgery in a direction it should never go.
Implicit inside the aim is also the intent of the surgery. When it is the total removal of disease and an anatomical restoration of the body, surgical outcomes seems to be the best and most aligned with the methods that get common discussed at conferences and in masterclass videos.
Next comes the risk. Being aware of the risk involved not just in a surgery in general but in every step, every dissection, and being cognisant of it can help avert a lot of problems. An awareness of risk, is itself a risk mitigation procedure.
A study published in the Annals of Surgery evaluated surgeons' self-assessments of their technical skills and found that those with lower peer-reviewed ratings had higher complication rates after bariatric surgery. This suggests that increased self-awareness among surgeons regarding their technical proficiency and potential risks may contribute to better surgical outcomes.
But no one is perfect. Some risk will always creep in and we must learn to manage it. But what now drives the surgical outcome up, over and above these factors is our learned excellence for conducting the procedure.
So the goal of the rest of this newsletter is not to give you insights into something we don’t already know, but rather to reorganise our thoughts, and look at the mathematics of surgery.
Alright, let’s begin. I am going to take you through the procedure of colon mobilisation in a case of deep infiltrating endometriosis or DIE. With each stage, we’re going to observe how we take this equation of aim, method, risk, wisdom, and excellence, to carve out the best outcome for a patient. A regular life.
The fundamentals of the surgery are simple. We try to isolate all critical organs, vasculature, and nerves, and remove all the nodules.
Colon mobilisation
The aim here is to free the colon of adhesions. The method is fairly straight forward, we use a harmonic to dissect and create planes in the tissue and gradually free the colon. Beginning laterally and moving forward. Our collective wisdom has taught us to always begin with this step. The human body is a congested house, the pelvis, even more so. Hence creating room is critical and this helps us do that. The risk that we run here is causing injury to the colon which could mean months of post-op recovery. How do we counter that? The last element of our equation.
Excellence in colon dissection is attained when we learn to differentiate between the fat of the colon and the fat of the lateral pelvic wall. Dissecting precisely along this line ensures we aren’t injuring any major vasculature.
And just like that, we’ve created some room for further dissection so we move to the next tricky bit. In a subsequent edition, we will talk about the next step, that is Ureterolysis.
But what’s important to see is that you can take any part of a procedure and view it from the lens of our five essential elements.
Aim, method, wisdom, risk, and excellence. Once we have that in mind, it becomes a matter of checking if the aim and intent of the surgery is sufficient and intact; if the method correctly achieves the aim; whether wisdom teaches us anything about that method, and at last, what can we really do to bring excellence into this step.
Every single dissection or firing of a scalpel can be broken down into these 5 steps. At a micro level, when performing very small steps, the aim and the method more or less become constant. You’re slowly trying to dissect in a certain area for example. But the risk continues to vary depending on where you are in the pelvis, what the surrounding and the underlying organ are and so on. And with each varying risk, you have a shifting goal post of what derives excellence.
Of course, you can’t be thinking of equations in the middle of every surgery. That’s not how this works. This isn’t an intro-op tool either.
We like to think of mathematics of DIE as a reflection tool. It’s to take what we did, and look back on if we could’ve done something better, if we could’ve made some improvements to what we did.
It’s a tool for continuous improvement.
That’s all for this week. We will see you next week with the Mathematics of Uretrolysis