The First Principles of Bipolar Electrosurgery
Breaking down the basics of how a bipolar works can help you dissect tissues more effectively
It is both stressful and annoying to find yourself in the middle of a rather complex endometriosis surgery and you notice some oozing that you just can seem to be the source of. Novices are even known to loose their patience some times.
More often than not such bleeders arise due to impropper coagulation and sealing of dissected tissues. Depending on the patient’s condition and any existing co-morbidities, such bleeders can quickly snowball into an intra-op complication.
Which is why we’re dedicating this edition of Endometriosis Weekly to understanding exactly how a bipolar scalpel works, and what impacts its performance. We will be looking at tissue contents and the impact of heat on different types of tissues that gives varying coagulation behaviour.
To being, let’s kick back almost 95 years when William Bovie’s invention and Harvey Kushing’s neurosurgery laid the foundation for what we ubiquitously use as a ligation and sealing technology in operating theaters today. While the invention was revolutionary, it wasn’t until 1998 (almost 75 years later) that we saw the first commercially available electrothermal bipolar vessel sealing instrument.
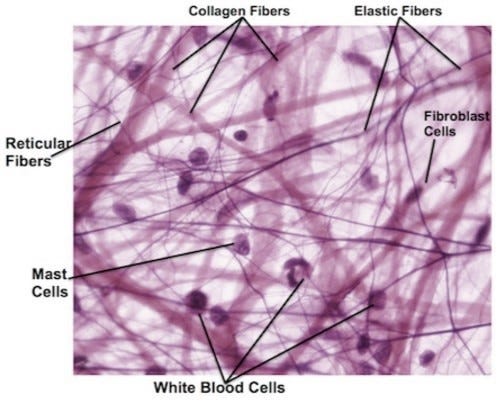
So let’s begin by understanding the principle of sealing - two sets of factors control it - physical factors include compression, heat, and time, and biological - collagen content, elastin content, and water in various tissues.
Vessel Content Considerations
In order to effectively use the controllable factors, we must understand how the uncontrollable facotrs vary.
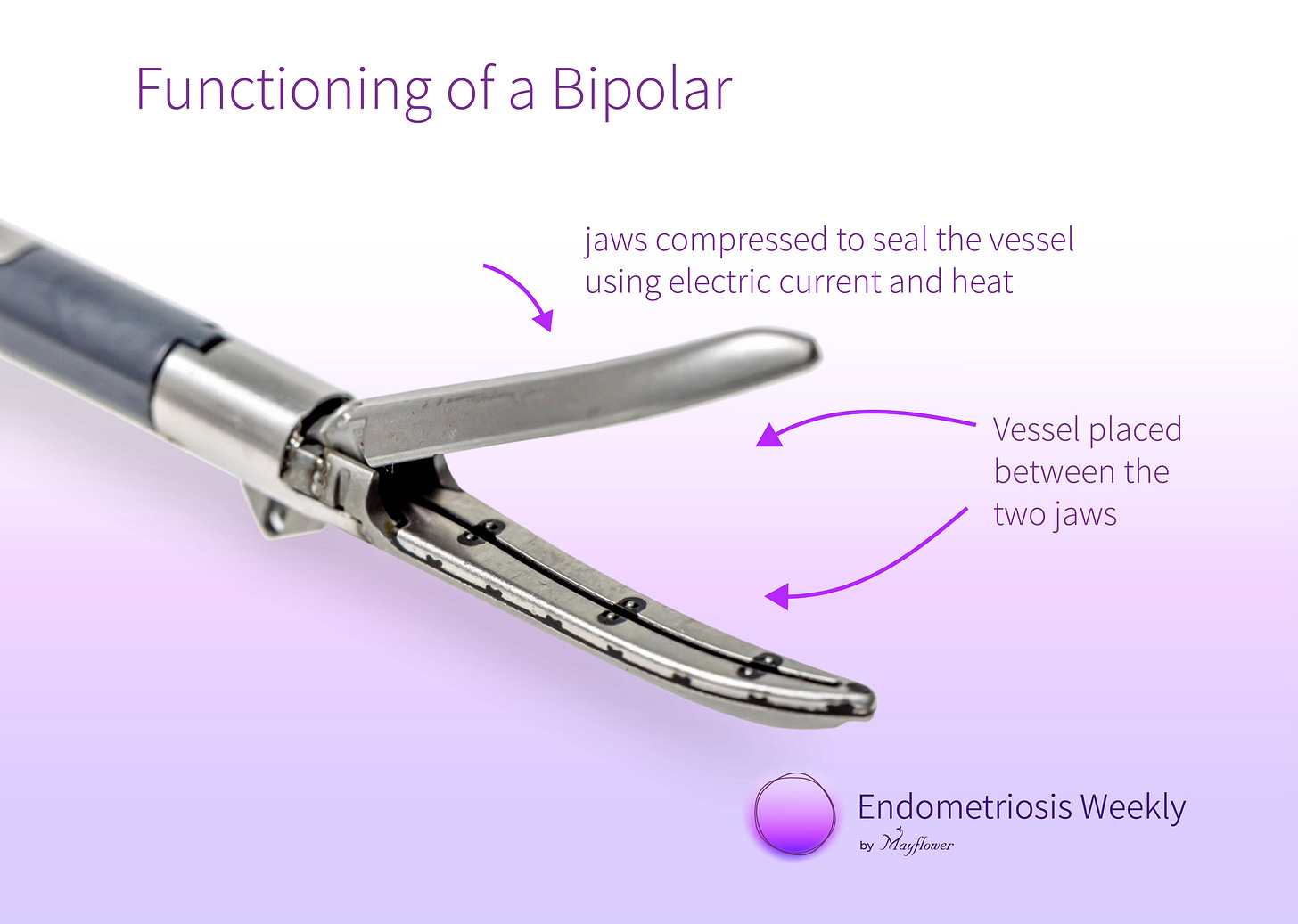
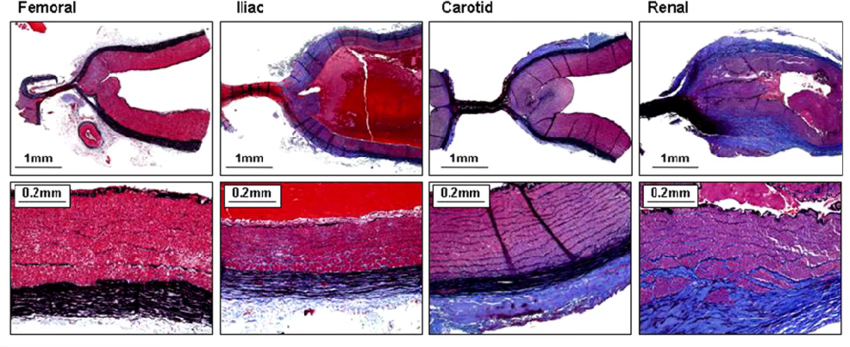
Each vessel that we encounter in the pelvis has some collagen fibers, that give it structure, and some eastin fibers that give it strength and resilience. When using a bipolar, we place the tissue between the jaws of the probe.
Once the probe is activated, current passes through the tissue and it gets cooked leading to coagulation. The collagen content of the vessel wall, relative to its elastin cotent, directly determines how strong the seal will be. Or in other words, how high the pressure it can sustain will be.
Collagen gives the vessel strength, and structure while elastin gives it the ability to increase or decrease in size based on pressure or other factors.
Here’s a diagram that explains how across various vessels, a changing collagen-elastin ratio impacts the mean aterial pressure that the sealed vessel can hold.
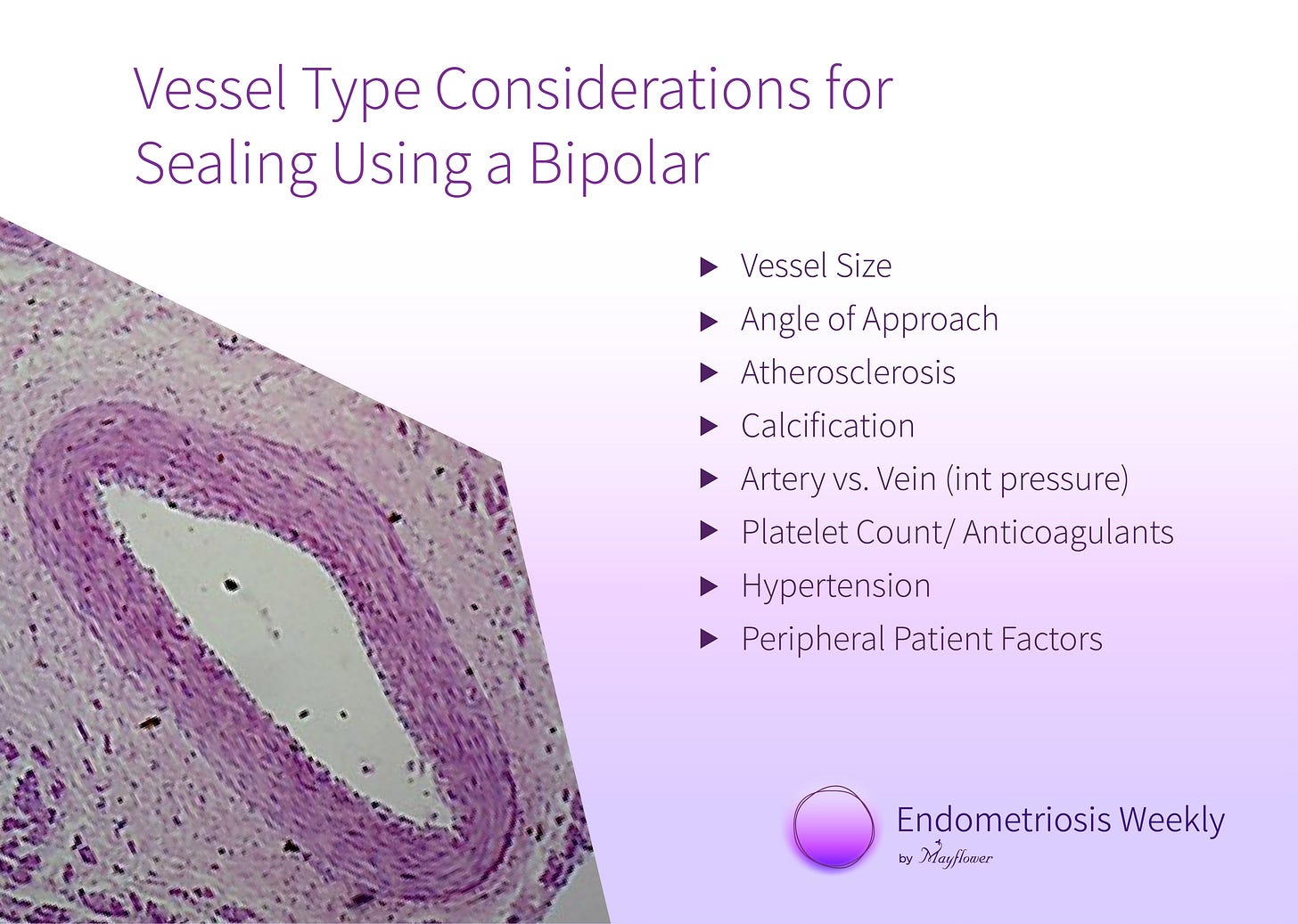
Vessel Type Considerations
But that’s not all, there are several vessel properties that affect the quality of seal and the eventual burst pressure. For instance the size or diameter of the vessel, the angle of approach, calcification, atherosclerosis, type of vessel, the patient’s platelet count, hypertension and more.
Another interesting but counterintutive fact is that smaller vessels hold up higher burst pressure compared to larger vessels.
It’s counterintutive because one would thing that larger vessels have more collagen and a stronger seal might get formed, however, it’s the smaller vessels where the the cross section to circumference ratio gets higher and therefore you get a relatively stronger seal.
Angle of Approach
The Angle of Approach is another aspect to consider, especially since it’s almost always under our control.
A perfectly perpendicular approach will always provide with a reliable seal, as opposed to a transverse approach.
A transverse approach increases the net cross section of the vessel that is within the jaws of the bipolar thereby increasing a chance of failure due to high fluid pressure.
Other Tissue Hinderances
Besides fat, tissues like muscle, lymphatics, and solid organs also hinder effective coagulation of the vessel.
Fat, due to no collagen, and low water content weakens the seal. Arteries with fat deposits therefore don’t necessarily form good seals and additional measures like clips where applicable, should be taken
Muscle fibers have a highly varying collagen content and therefore when overlaying a vessel might impact the nature of the seal formed.
Lymphatics and solid organs also weaken the seal owing to similar reasons.
The tool is like an extension of your our hands. Familiarity with how it behaves under different conditions, how different tissues feel different under it, can all aid our awareness in surgery and help bring out better outcomes.
We hope this issue helped add to your knowledge bank and your surgical confidence.
Until next time!