There’s a popular story about a doctor and a mechanic that often makes rounds at parties. If you haven’t heard it, allow me a minute. It’s very entertaining.
So the story goes something like this.
A doctor’s car breaks down in the middle of the road. He calls a mechanic. The mechanic comes and fixes the car.
As he’s wrapping up, the doctor pays the mechanic his fees and a tip, thanks him for the service, and starts to walk towards the car.
That’s when the mechanic says, “You are a doctor right? You and I do the same thing. If an engine doesn’t work right, they call me, when the heart doesn’t work right, they call you…”
“Yes. So what?” the doctor asks, waiting for the mechanic to get to the point.
“Why is it then that I only get paid $50 for doing it and you’re paid $15000?”
The doc looks at him, takes a pause, smiles lightly and says, “Try doing it with the engine running” And then without waiting for a response, drives away.
The smug doctor is not what’s important here. At least not for us. What’s important is the realization that we must fix engines while they’re running. Often replace entire parts without letting the car shut down. That’s a big responsibility. With some systems, this problem gets harder. But you would be too naive to this the engine is only a metaphor for the heart.
Several other systems rely on continuous operation, the renal system being one. This is also why endometriotic involvement of the renal system, especially the ureter and the bladder, causes such complex and often urgent needs for surgery.
Today, let’s take a look at how we fix endometriotic involvement of the bladder, of course, while keeping it running.
At Mayflower every surgery is unique and every case takes a village to solve. A tailor-made approach to every patient is central to our approach of surgery. There are no cookie cutters.
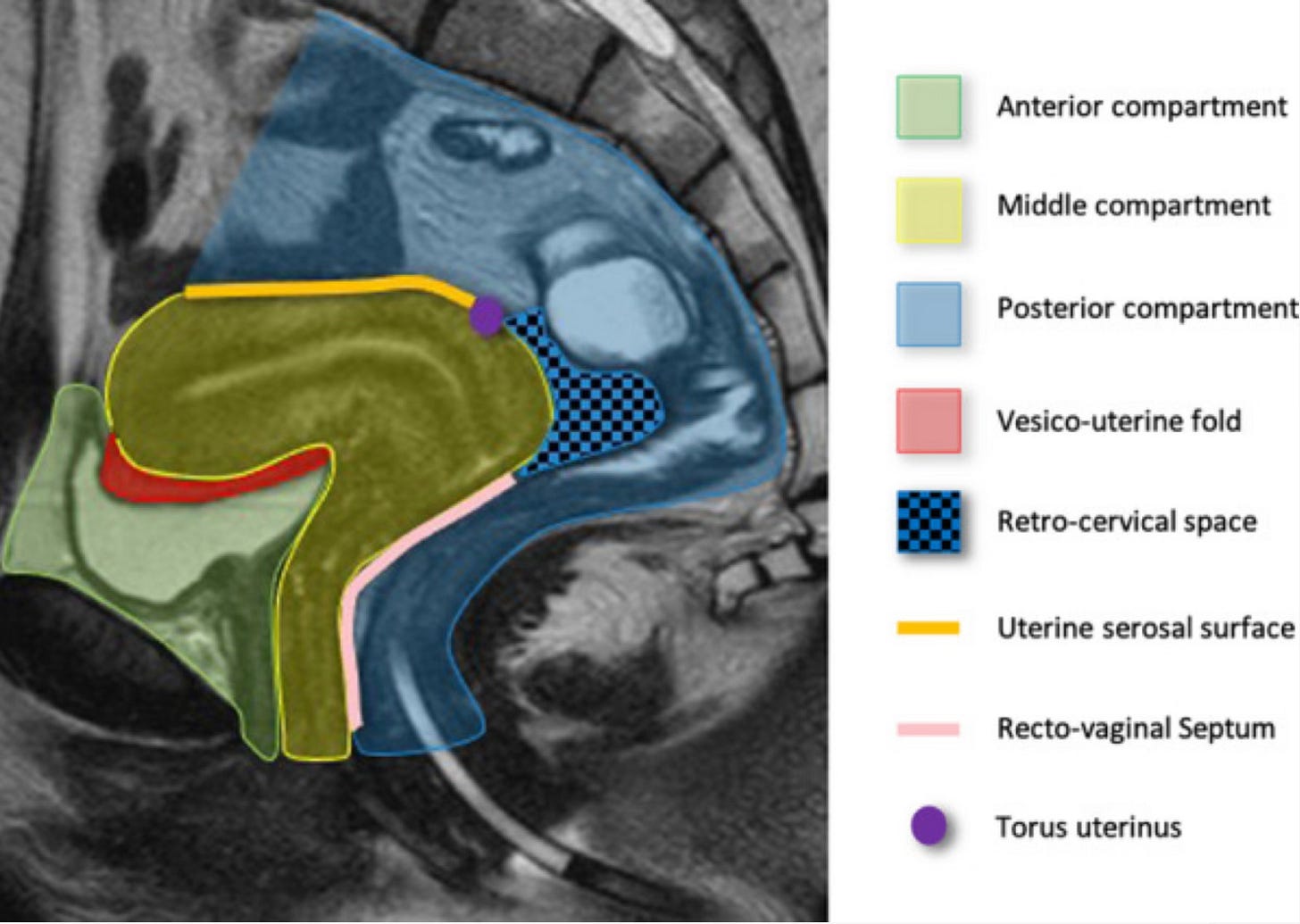
It begins with an MRI scan, which in conjunction with an ultrasound helps us thoroughly map the disease. We use an extensive compartment based format for disease mapping focusing on each region separately and in great detail so as to not miss any instance of occurance.
This map is key to defining critical aspects of the surgery
How widespread is the disease?
What procedures are likely?
What specialists do we need to involve?
What are the risks involved and how do we inform the patient about them?
What equipment do we need?
Restore - Not Cure: Building the Surgical Plan
At Mayflower we strongly believe that most of the worst impact of endometriosis can be reversed simply by restoring a pre-disease anatomy of the patient. This means that our approach to surgery is conservative.
If it’s not broken, we don’t fix it.
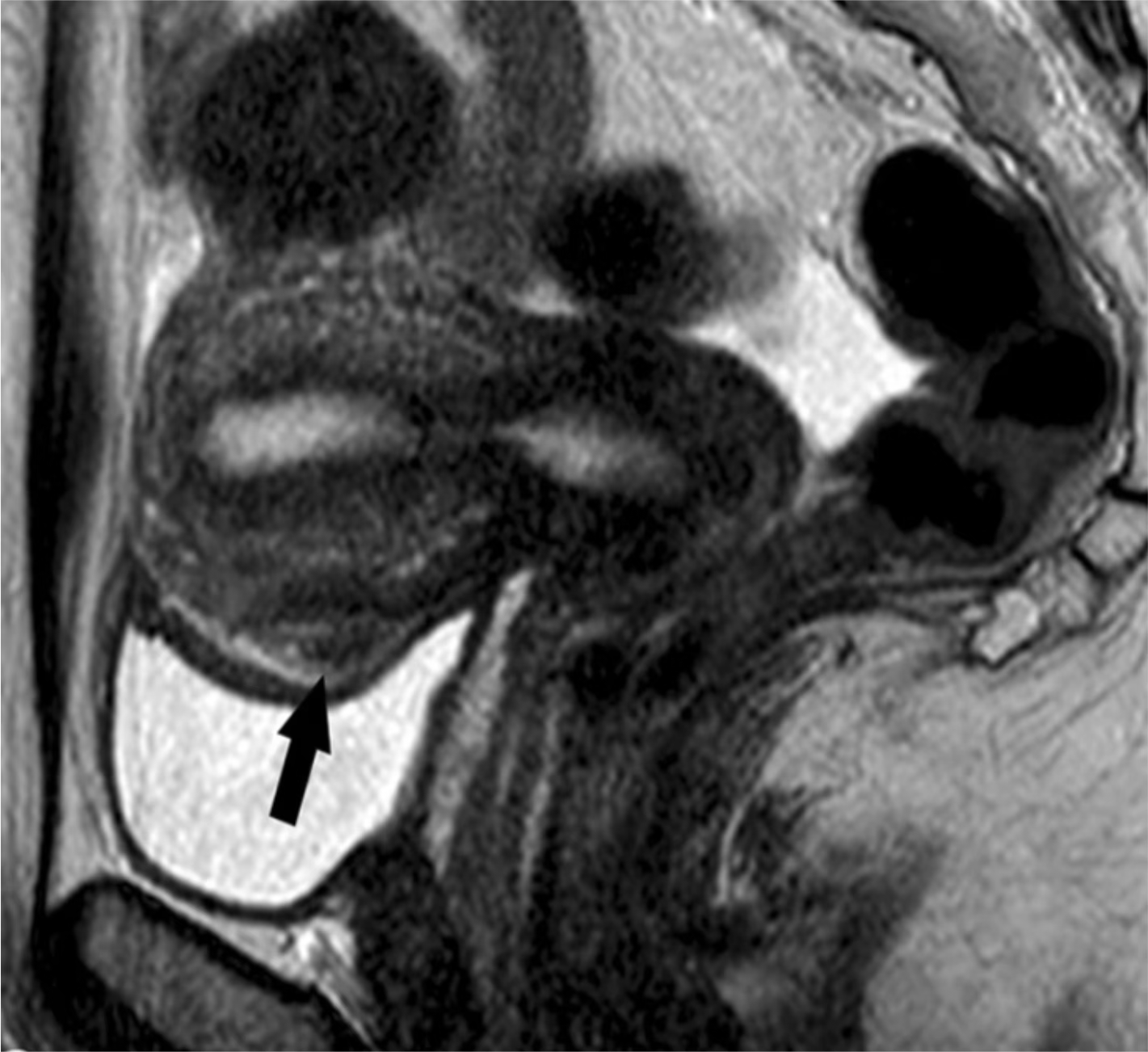
In the case we look at today, there exists a bladder nodule, but the mucosal layer of bladder is not involved. Which means the involvement is extrinsic and that should be considered good news.
On an MRI it typically shows up as leison on the bladder wall.
Pro Tip: The report must specify whether an obliteration of space exists or not. This has an impact on the surgical plan, specifically in terms of isolating the bladder.
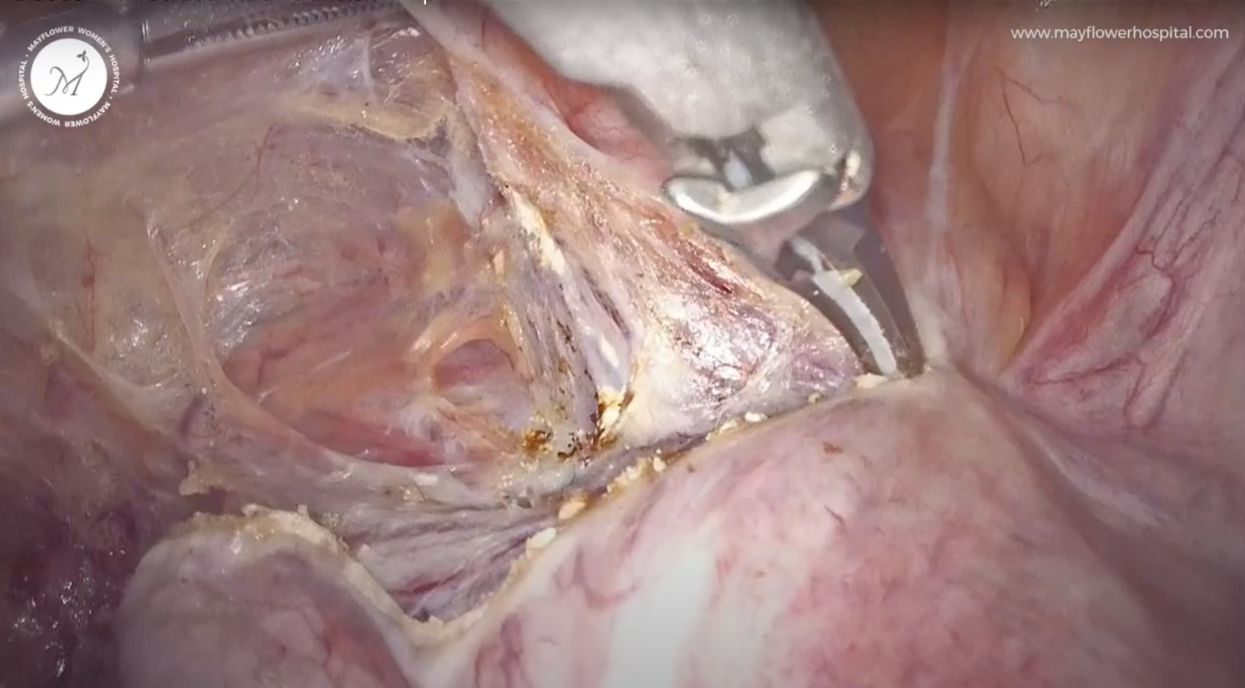
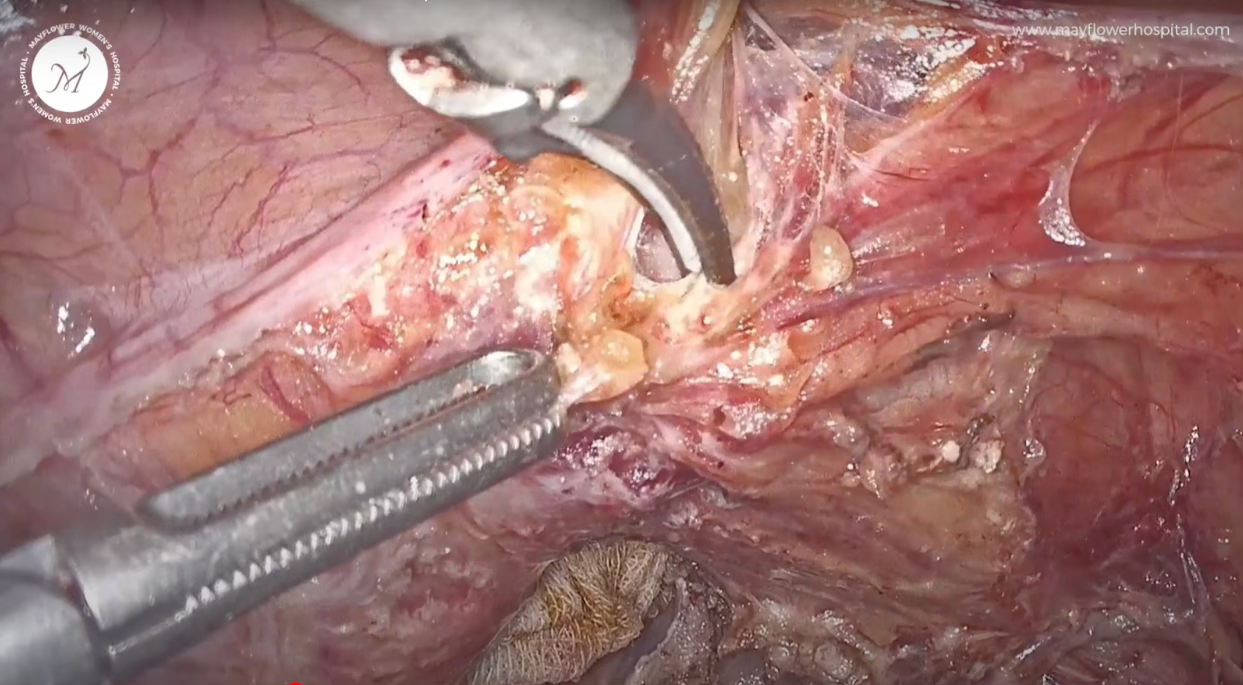
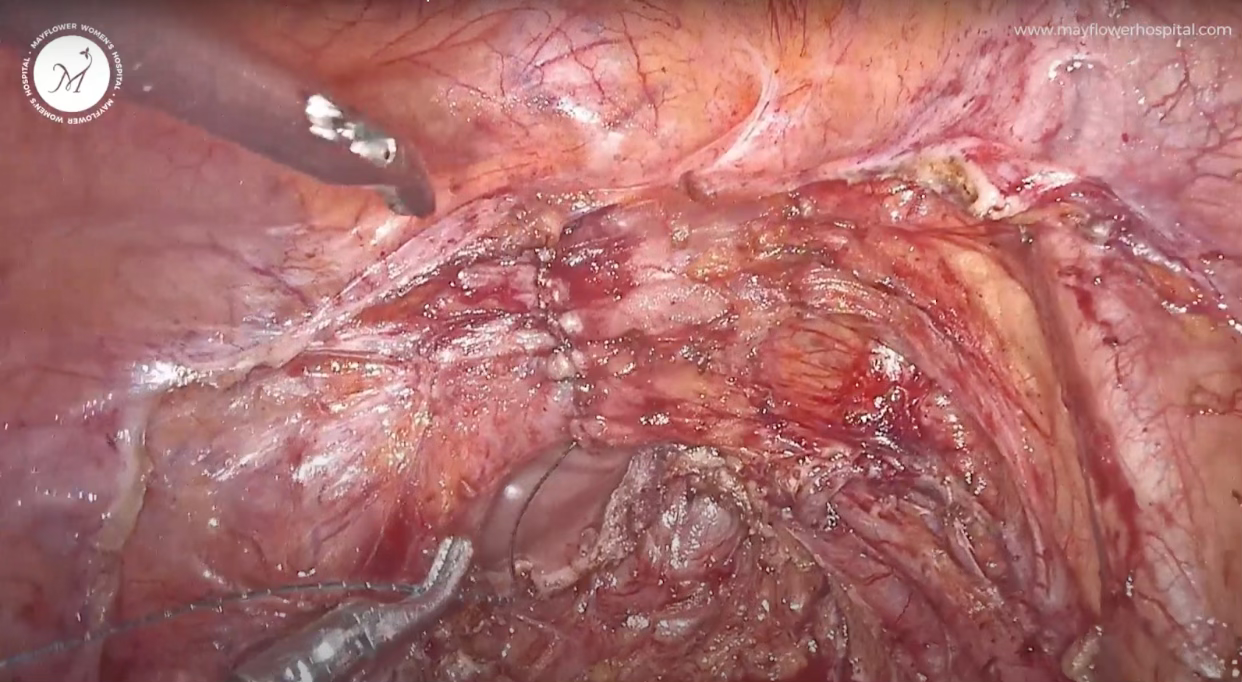
Once we’ve dealt with all the other nodules in the space, we come to deal with the devil. A process that begins with identifying the vesico uterine fold.
How to do that well? ProTip: Remain between two planes. One layer goes to the bladder and the other slides over the cervix and vagina. While dissecting, stick to the line in the middle. Visually we can identify vascularity within each layer that goes to the respective organs, and what’s left in the middle is our plane of dissection
Once the Utero-Vesical fold is dissected, TLH is performed, opening up the space and giving us a clear view of the nodule. This is when we first get to inspect the nodule in its entirety. We feel the nodularity and at the same time hysteroscopically reconfirm that there is no mucosal invoplvement.
Proceeding with the surgery, our first aim is to dissect fat surrounding the nodule. This is achieved by doing a fiber by fiber dissection. If I had a penny for every time I said fibre by fibre, you and I both could’ve retired by now and spent a Wednesday fishing in a European lake. But the world doesn’t work like that. Fibre by fibre however, is still just as important.
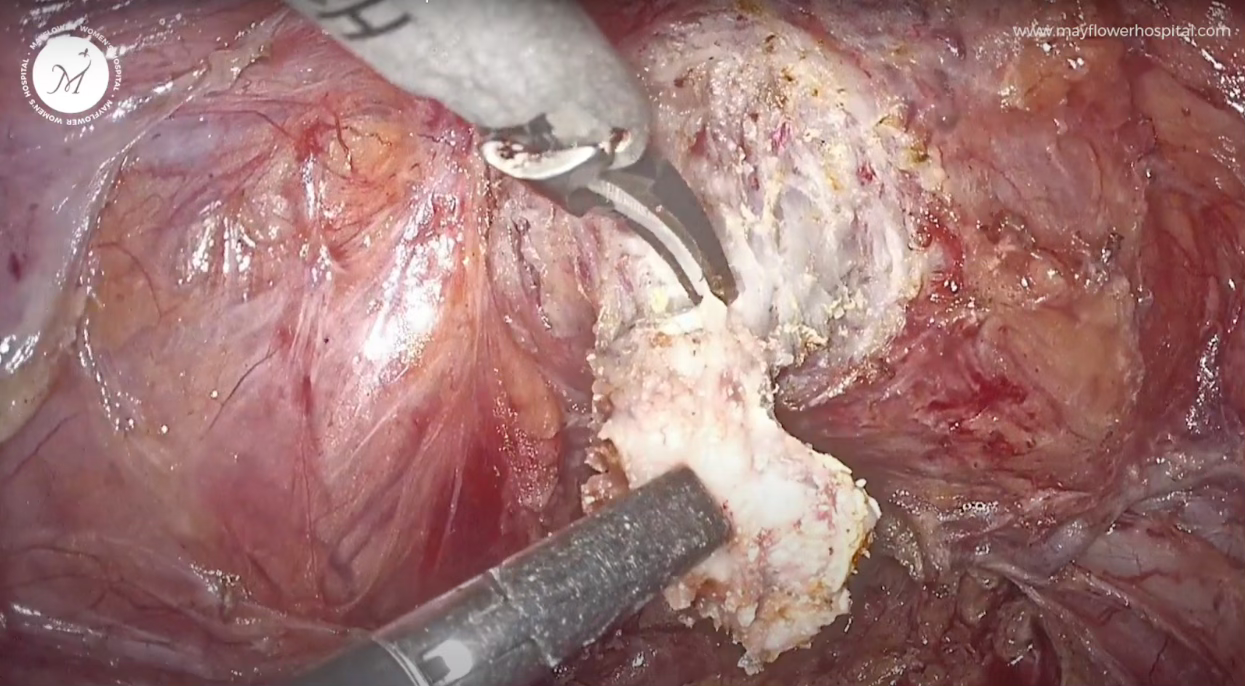
We dissect fibre by fibre, denude the fat around the nodule and then dissect off the nodule from the bladder parenchyma.
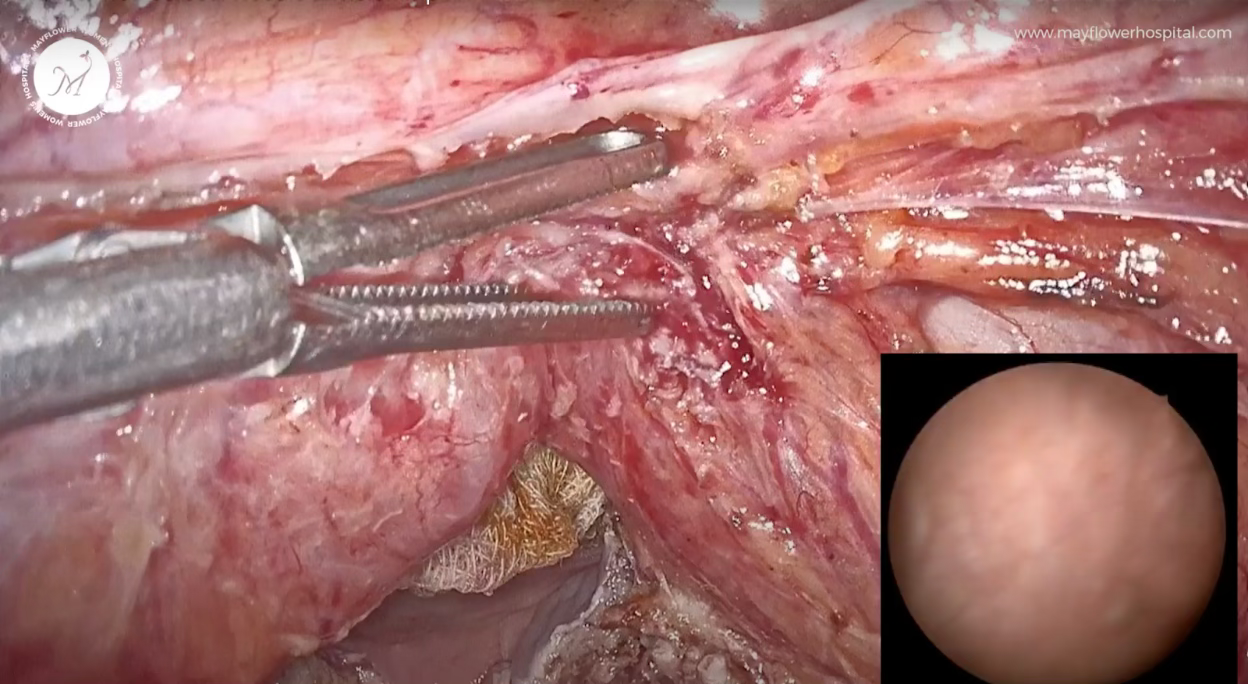
As we dissect fiber by fiber, at each activation of the ultrasonic scalpel we feel the nodularity. It’s an odd thing to say but there’s no better way of saying it. At first you feel that there’s the tissue, and then the probe’s tip, and then the shaft, and then all the way on the outside, your fingers on a trigger, but even then, the human mind has a beautiful way of learning.
As you perform more and more dissection, the impact of a probe’s activation, the cavitation, CO2 flooding in, coagulation, all start to become apparent to you through the probe. If you look closely, you can tell what tissue you’re holding, and that becomes the way of sure shot success.
In doing so, we always make sure that there is no diseased part left behind, but at the same time we do not want to open the mucosa of the bladder either, as its not involved. This is when fixing it while keeping the engine running, becomes real.
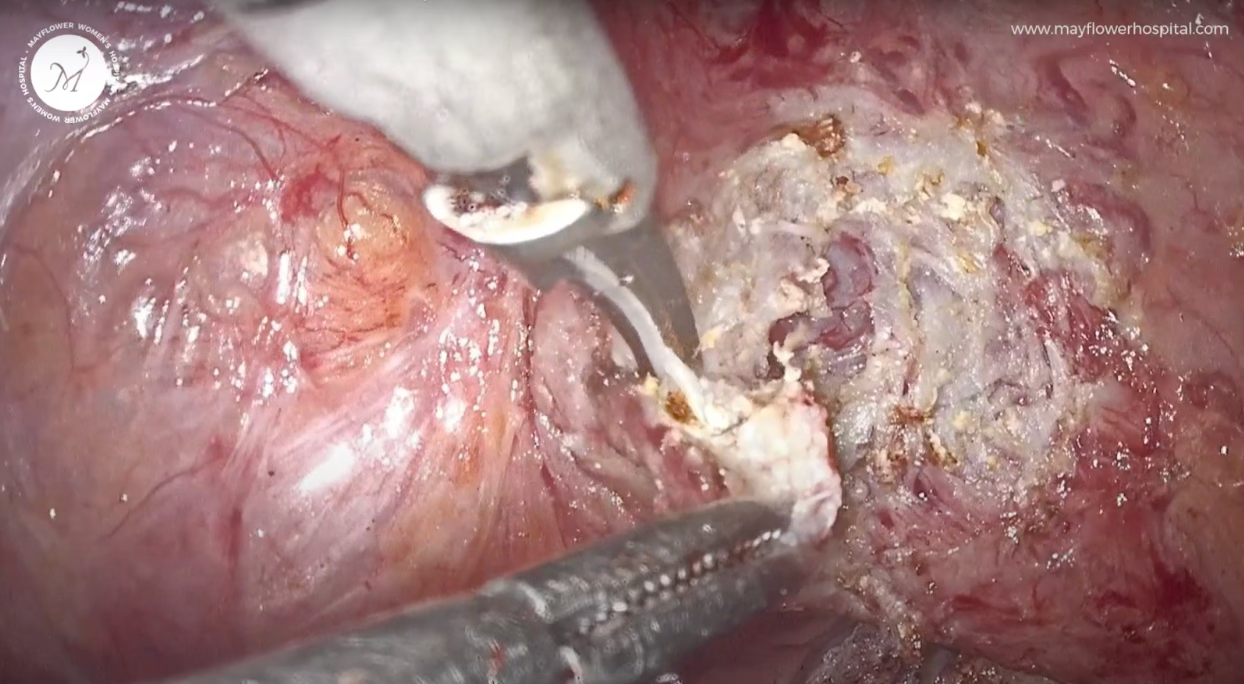
Next, we inspect the surrounding margins, and see if there is any nodule left behind. If so, we remove it with the same surgical precision.
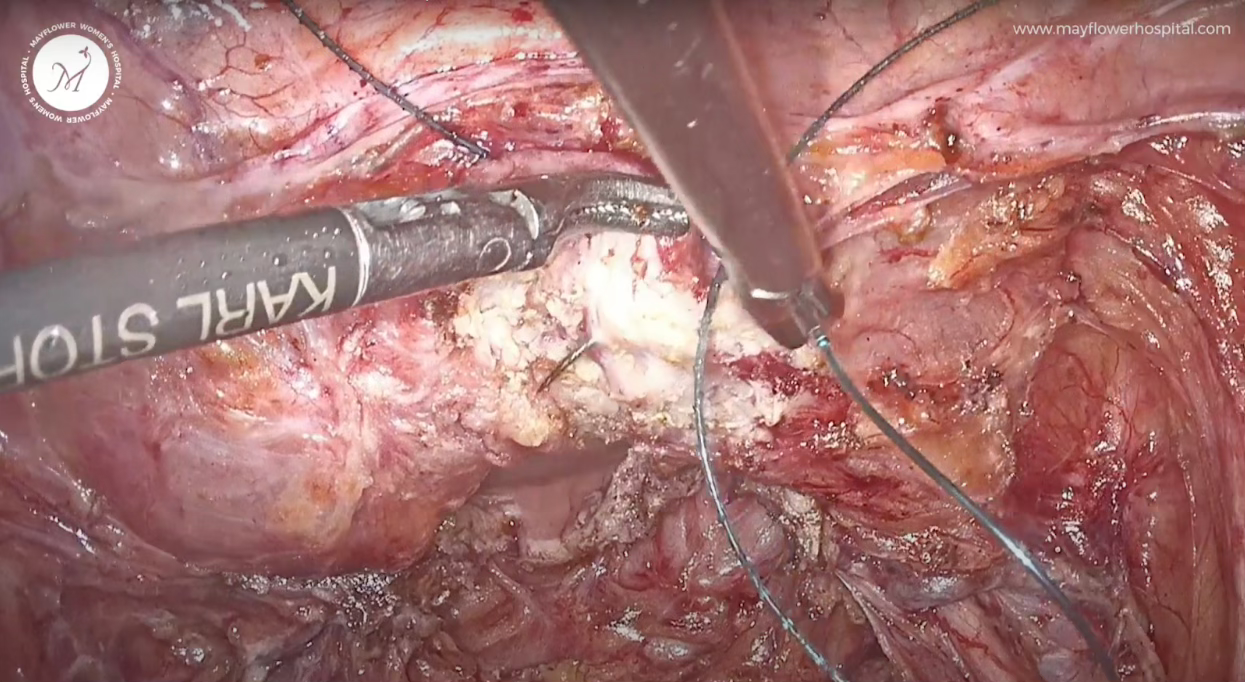
Once we’ve removed all the nodules, we move to suturing.
We close the defect in vertical fashion. The suture used is a 3-0 barbed suture.
While penetrating, we take a deep sero-muscularis section. A good tension free approximation of surfaces is the goal of sutuing
Amd this is the end view. We started the case with deep infiltrating endometriosis, removed all the diseased plaque; gave a patient endo free bodily tisues, good quality of life, no pain, and almost no genito-urinary tract symptoms post recovery.
That’s what one can achieve with an anatomy conserving approach. It’s easy to treat surgery as a craft project, but thinking of it curative, as though it were a process of finding purpose, and delivering a second chance at life, makes us act and evaluate differently.
Hope this editing helped you understand the procedure and the mindset. We are always happy to take questions on ew@mayflowerhospital.com
Until next week!









Nicely achieved end result and nicely penned down! Simply superb