Happy New Year! Some of you might still be on vacation enjoy either the hills, the beaches, or just your very beautiful and carefully detected living rooms which is why today’s issue will also keep it light, ruminating, and exciting.
Today’s edition covers 5 bold predictions we are making for Endometriosis in 2025. These are both in preparation for the days to come, and a learning from everything we experienced in 2024. So let’s get right into it!
1. Increase in Endo Incidence Rate
One of our first predictions is that an increasing awareness of endometriosis and its types within doctors and patients will lead to a greater reporting of the disease owing to a larger number of more aware patients.
A number widely reported as 10-11% is likely to jump to 12-13% in the coming year.
More disease sounds like a bad thing but this is good. A greater awareness about detection, triaging, and treatment protocols will help aide women in leading healthier lives.
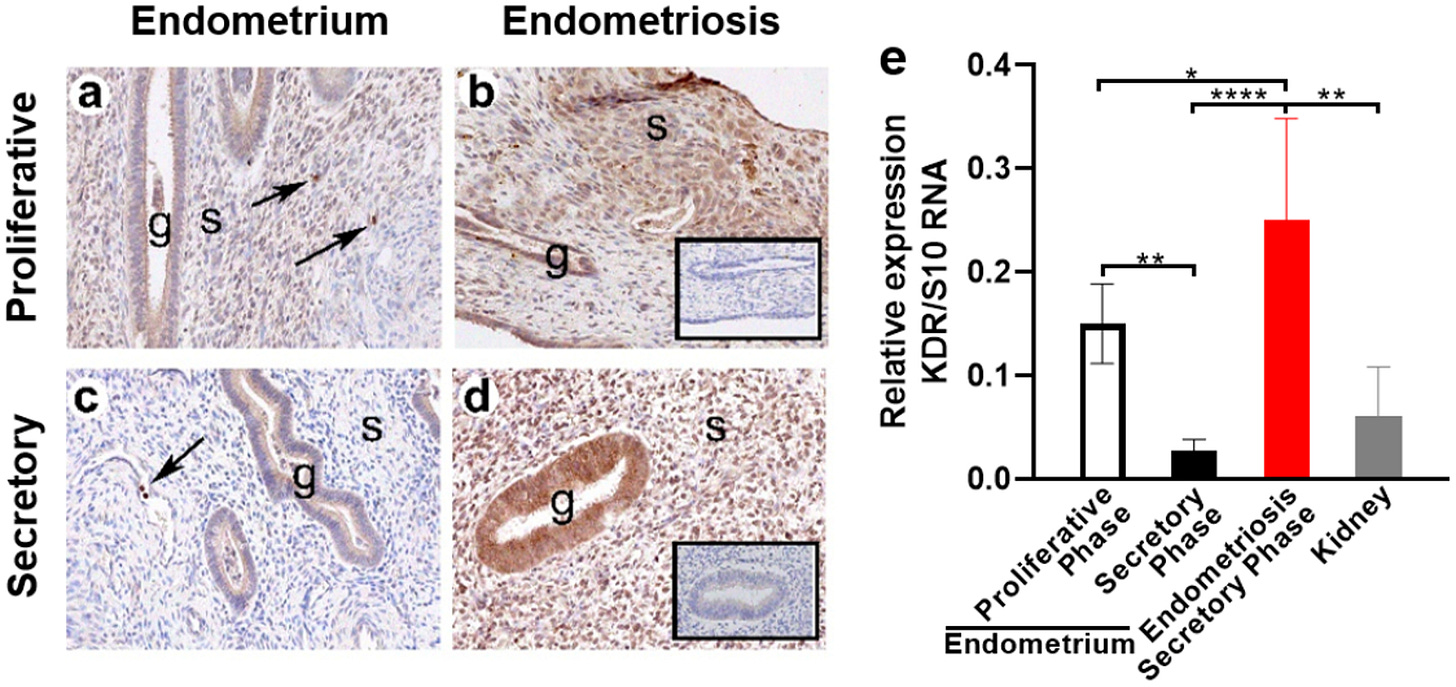
Breakthrough innovations like the 99mTc-maraciclatide imaging technique will accelerate early detection and make the handling of endometriosis much easier as more and more cases get caught at a stage where they are much more managable.

Plug: Mayflower’s New MRI Service
In a bid to make Endometriosis detection more accessible to people, Mayflower has initiated a remote MRI repoting program where gynecologists or patients can directly upload their MRI files on to a form on our website and have the MRI read by Mayflower experts holding extensive experience in disease mapping from the thousands of cases we’ve dealt with so far. You can access the form here
MRI reports come complete with specific markings for disease occurance and radiological observations of the likelihood of tissue type, space obliteration, and visible anatomical distortions.
Each MRI is extensively studied across 8 different compartments and landmarks within the pelvis to give the gynecologist a comprehensive understanding of the disease.
Alright. Back to the predictions now.
2. Medicine vs. Surgery: The Battle Continues
With an increasing number of advancements in both surgical imaging, dissection technology, robotics, and medicines that help manage active, passive, primary and secondary or peripheral prospects of endometriosis, the battle between medical and surgical management of endometriosis will thicken.
The cutting edge of medical management looks very promising actually. On the one hand studies about magnetic nanoparticles and their use for targetted treatment of endometriosis while on the other, we have non-hormonal theraputics that help target and kill endometrial cells. A lot of this research will come to the fore in the later part of this year.
Patients will largely, and understandably, choose non-invasive treatment sometimes even when they might be slightly less effective owing to the potential and very real risks involved with surgical treatment.
But it remains to be seen what the long term effects of new medical management might be. Their non-hormonal nature can help counter some effects of existing therapies but how they impact reproductive health, and overall anatomical normalcy of the pelvis remains to be seen.
Conjoined protocols of medical and surgical treatments combined to given total disease removal with anatomical restoration and normative reproductive health might still catch more steam.
We will see. We’re clearly biased towards surgery.
3. Ultrasonic Everything
As education advances, and a greater number of doctors engage in continued education programmes, devices in gynecological surgeries will shift.
The current landscape is predominantly bipolar scalpels and shearers but this will grow towrads a greater use of ultrasonic scalpels.
This will mean a general shift in how we perform surgeries and our average confidence on cuts and dissections. Ultrasonic scalpels generally give surgeons a smaller margin of error and therefore a more precise cut owing to the energy source being inherently non-pyrogenic and yet heat causing in nature.
4. Dawn of the Bots: AI and Robots will take over
Surgeons and radiologists might get some time off to sip on coffee and callously bithc about why cardiologists get paid more. 2025 is going to be the year where Robot and AI agents will start showing high effectiveness in assisting procedures involved in both detection and surgery.

Robotic surgeries or RALS (Robot Assisted Laparoscopic Surgeries) aren’t a new deal but with a shifting business model and leasing associated with per procedure pricing models will make them more accessible, especially for smaller units.
Historically, the high price of Robotic surgery setups (norht of 8Cr INR) make them uneconomical especially in single speciality centres and make widespread adoption in multispeciality centers a problem of training and development taking several years of cash flow to give a postive IRR.
But as the tide turns, and new business models like leasing of the machine and per procedure cost come into play, there will be a greater number of Robotic surgeries taking place.
When you put AI and Robotics together, procedures, especially the ones that deal with deep infiltrating endometriosis, will see more repetability and better outcomes owing to the precison. The only palpable and significant roadblock is the availability of ultrasonic scalpels within a robotic environment.
J&J, a leader in the field of ultrasonics would want to hold on to their technology, only making it available with their OTTAVA robotic system that is still in a trial phase.
But even if the system comes out in time, there is no garuntee that it will carry all of J&J’s latest laparoscopic tech. Take Medtronic for example whose Soniscion ultrasonic scalpel still isn’t available with their Hugo RAS robotic system from the last we know.
If the surgeon is highly skilled, Robotics are a step back in time because they don’t make the best technology available to the patient. But if the surgeon’s skills are limited, Robots play a HUGE role in making sure surgical outcome and post op recovery is better. So regardless of the technology available, we will continue to see more robotic offerings on the market.
In any case 2025 is an exciting year if you’re a tech enthusiast in medicine, and it’s a bad year if you don’t like change.
5. Leaner, Meaner, Quicker Teams
With an increased rate of automation entering the healthcare system and greater reliability on technology, the number of hospital staff required to attend to a given number of patients will go down.
1:4 is the golden ratio
A lot of existing literaure from around the world puts the staff nurse to patient ratio at 1:4. While intensive care units might still have strong reasons to stick to higher staff levels, day care and other stable post operative units might find it easier to move to a leaner team.
With increasing automation in vitals monitoring, remote patient analysis, drug administration, and record keeping, a lot of rote jobs in a caregiver’s routine might be taken out, making room for them being able to care for more number of patients simultaneously.
That’s it! Those are our predications for the rest of the year. Close to the end, we will evaluate which ones held water, and which ones fizzled out. Till then, there’s a lot of surgery to talk about.
As we step into the new year, here’s us wishing you find everything that you’ve been looking for.












Excellent Article. Refreshing to know that these newsletters do exist in India. The narrative is so simple and elegant, like applying ultrasonic scalpel to the writing. For non professionals, it's devoid of medical jargons, and that's an art in newsletter writing. Hopefully, we would see advancement in diagnostics/Bio marking technique for early stage detection of endometriosis in the coming years.