Peeping into the Dark Void : Lessons from 1000+ diagnosis for Deep Infiltrating Endometriosis
How MRIs revolutionised surgical planning at Mayflower for Deep Infiltrating Endometriosis surgeries
Welcome to the first edition of Endometriosis Weekly. If you’re reading this, you’re amongst the first people to become part of this ambitious endeavour to understand endometriosis. Our weekly newsletter has finally kickstarted and we intend to keep it going.
Looked at from the lenses of various specialities, this newsletter is aimed at helping you discover something new about the disease each week with
academic deep dives,
case studies,
expert opinions,
and occasional poetry.
This newsletter is meant to be a thought starter to the never ending science of endometriosis surgery.
Oh also, the last thing we want to be is boring. 🤮 It’ll be our constant endeavour to keep things fun 🎉 while also delivering serious value 🔬. If you have any thoughts, questions, opinions, or brickbats, please send them our way on ew@mayflowerhospital.com. We read every last email that we get.
Alright, let’s dive right into today’s edition.
The dark is always scary.
Not because we don’t know what’s in it, but because we are driven mad by the anxiety of everything that could be. It is not the knowledge of a big threat that causes fear, it is the lack of knowing. The more light we throw at things we don’t know, the lesser our fear. No matter how big a challenge the light reveals.
Diagnosing endometriosis has been historically hard on various levels. On the level of symptoms, one can only so much as indicate the possibility of endometriosis. Especially with cases of deep infiltrating endometriosis, the challenge of misdiagnosis causes severe distress. What do we do then?
Finding the Gold Standard
Let’s go back to school.
“What is the gold standard for diagnosing endometriosis?” you’d ask a group of gynae residents and the brightest among them would say diagnostic laparoscopy. That’s a great answer. It’s also probably a right answer. What’s better than to see with a naked eye? (almost). But as soon as you accept that answer, you are also hit with a barrage of problems:
Surgery is complicated,
surgery is difficult,
and not everyone has the resources to go through with it.
And all this on a mere suspicion?
Sounds perilous if not egregious.
Also, what about the infiltration? You can’t see what you can’t see.
And for a patient who walked in with period pain, anaesthesia is the last thing they want to smell
Which is why it isn’t a surprise that Carol Overton and others in the Atlas of Endometriosis write that nearly 27% of symptomatic women go with undiagnosed endometriosis for nearly 6 years. That’s long enough for the disease to warrant a significant diagnosis.
Vigilance comes at a cost. There is a financial and emotional cost to the patient, and there is a cost of accessibility to society. And yet in retrospect, vigilance always feels necessary.
🔍But we’re near certain that symptoms alone, regardless of their detail or concurrence, are certainly not diagnostic and only point us towards endometriosis.
Which is when we come to imaging. An ultrasound is a gynaecologist’s most handy tool. Almost like an extra eye that lets you look beyond what is visible, albeit with much less clarity. The technology continues to improve year on year and we’re able to see better, however just as fast as we enter with hope, is about as fast as we are met with limitations
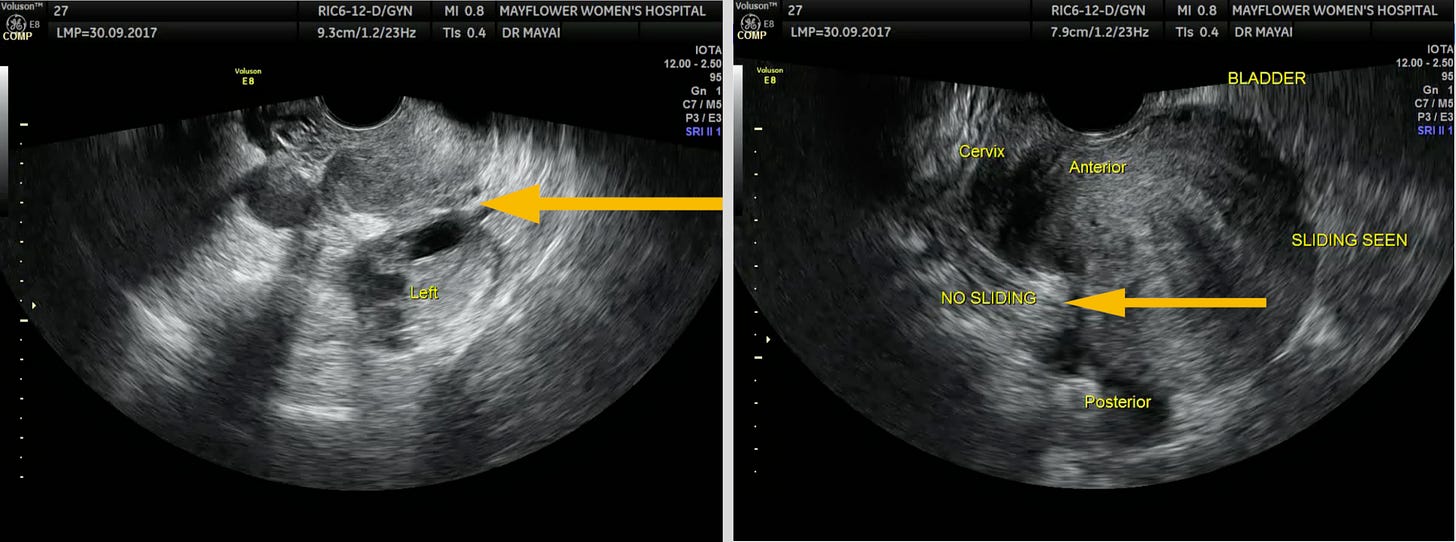
USG’s biggest benefit is availability. It’s a point of care instrument and owing to its wide range of applications, every gynae has one. Its second biggest benefit is live imagery.
Being able to move the TVS probe to observe sliding between the organs, might be the single most distinctive feature of the technology aiding in an early detection of adhesions inside the pelvis.
But USG can only go so far in determining the true extent of the disease. While it denotes the presence of endometriosis, it doesn’t help us accurately map the most damning feature of the disease. It’s infiltration.
Infiltration in Endometriosis is one of the key reasons the diseases becomes dangerous. Causing strictures in ureters and colons, invading entire peritoneums, and if one is out of luck, travelling north to more organ systems.
It is also this invasive aspect of the diseases that requires surgical planning. How far into the colon has it invaded? Can we handle it with rectal shaving alone? Will we need to do a disc excision? My god, do I have to do a resection surgery?
God has an answer
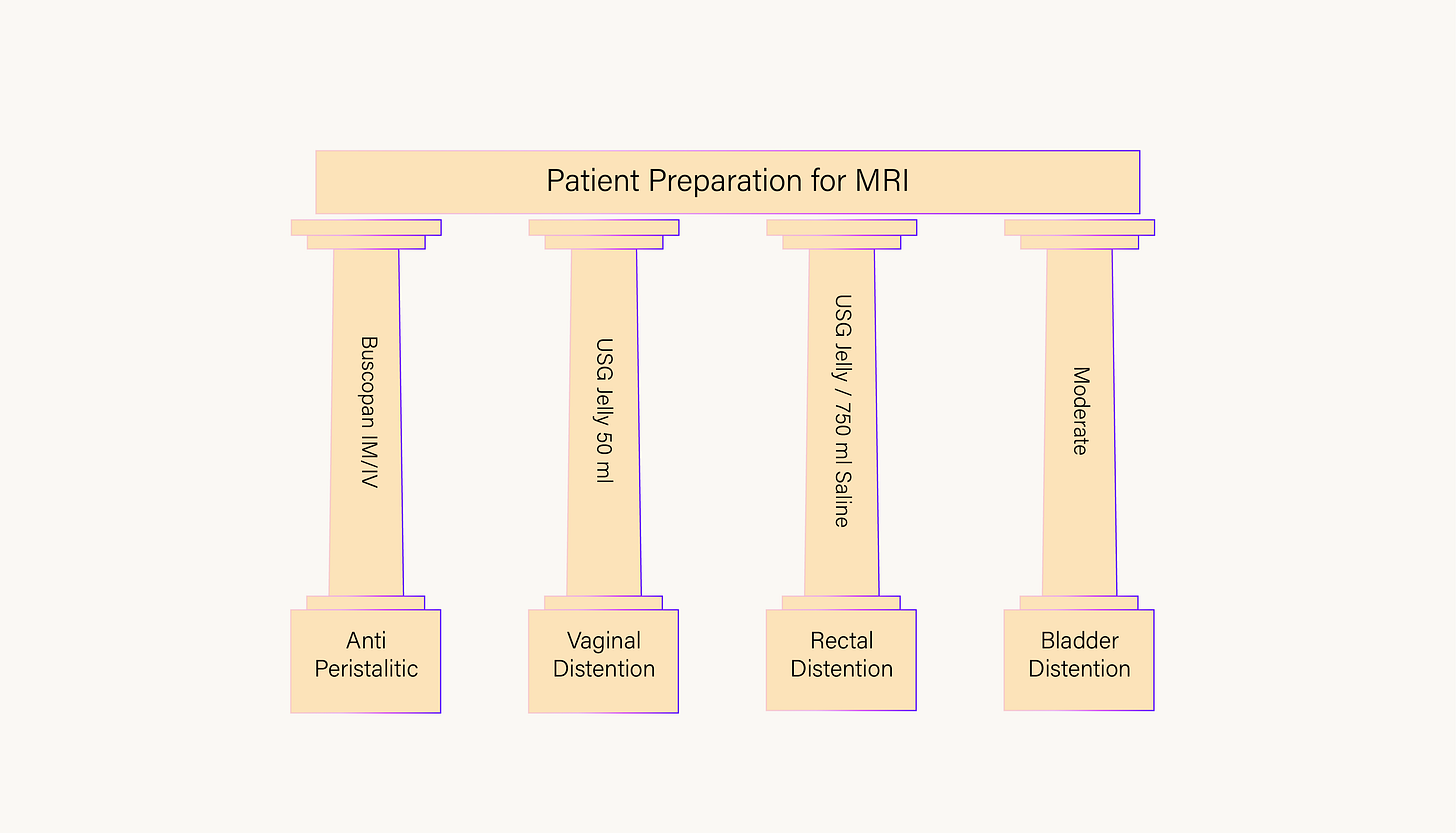
The quality of output, usability, and applicability of any form of imaging is determined significantly by the setup. While a radiologist adds maximum value at the time they help point out endometriotic lesions or nodules in the imagery, this interpretation is aided in large parts by the correct patient preparation. Conversely, bad patient prep leads to often inconclusive results.
There primarily are 4 pillars to great patient preparation. These include rectal distention, vaginal distention, bladder distension, and halted peristalsis. Here’s a figure that explains it in short but certain terms
Over the last several years, Dr. Jay Shah and team have worked very closely with us in building the best practices for conducting and MRI. Dr. Shah’s lecture on MRI in endometriosis is a thesis on these best practices and I strongly recommend you catch it whenever you have a chance.
For the purpose of this newsletter, we will focus on the broader aspects.
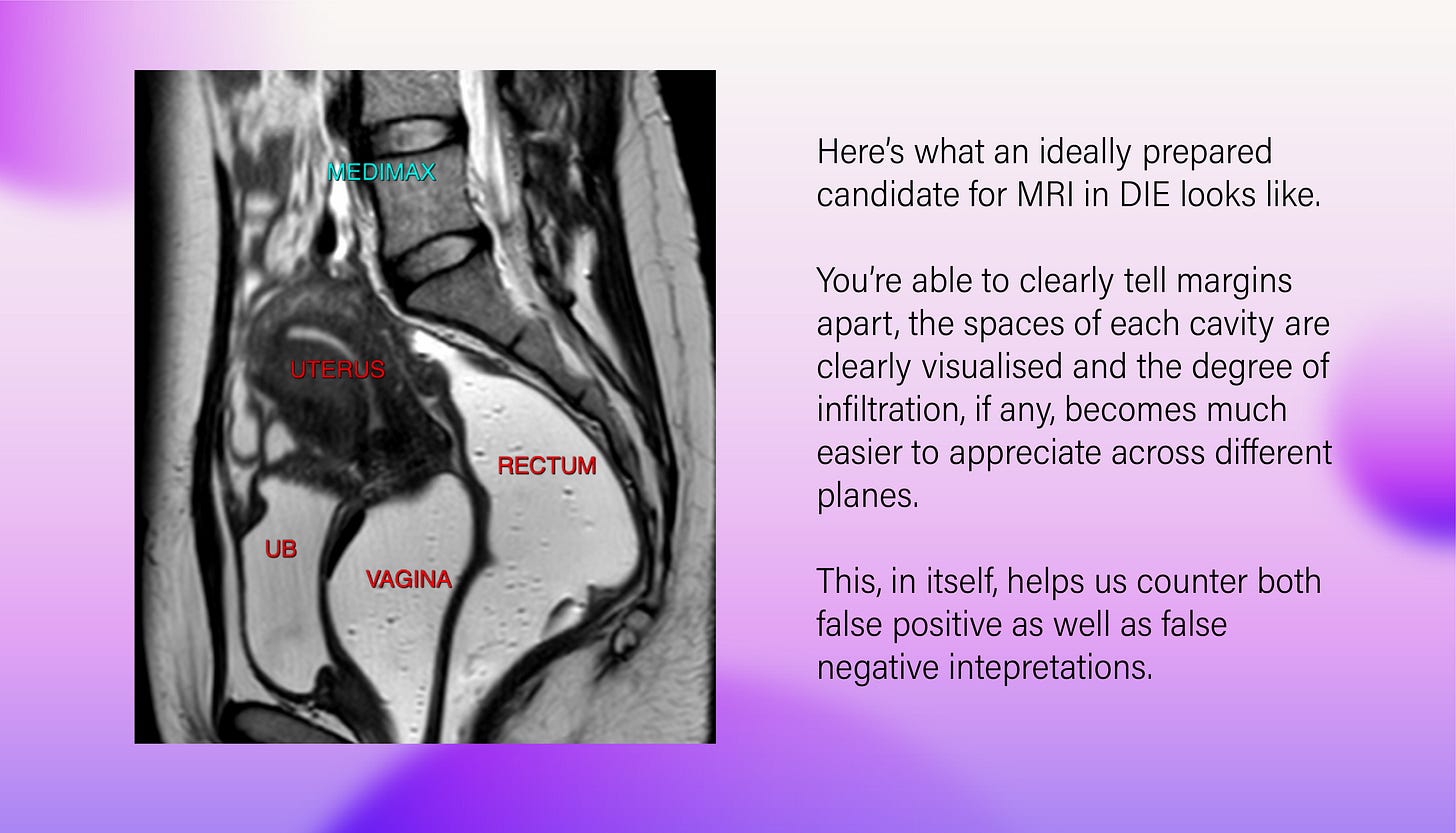
Once the setup is right, MRI can provide us incredible details about disease involvement and the level of infiltration. This becomes most useful in our pursuit of detecting infiltration of DIE in various cases.
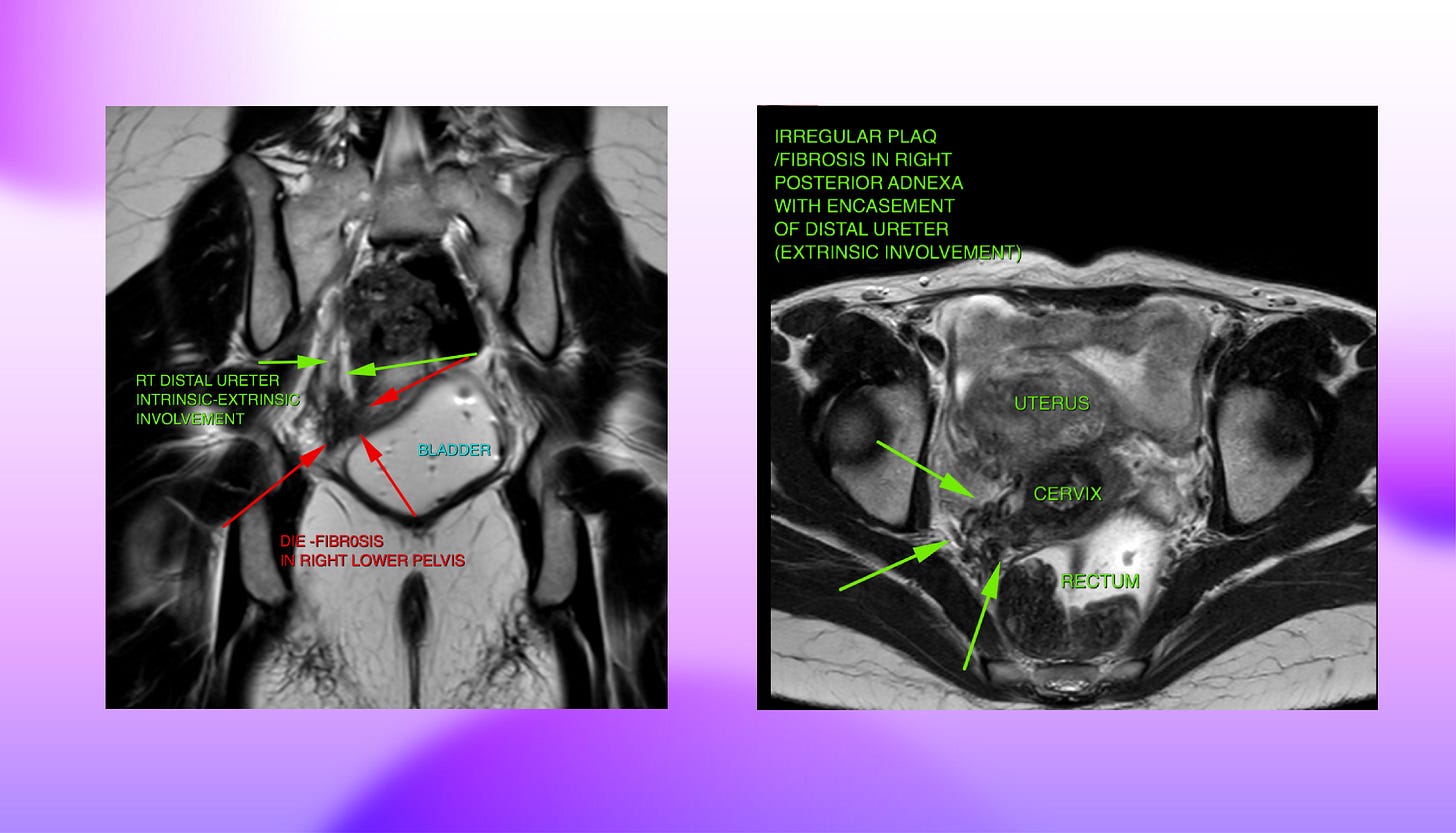
Take the ureters for instance. Observing irregular plaque or fibrosis in the right posterior adnexa in this instance of a T2 weighted axial slice shows an encasement of the distal ureter indicating extrinsic involvement of the ureter. This type of involvement typically results in tethering and angle deviation for the ureter. Whereas another T2 weighted coronal image shows both intrinsic as well as extrinsic involvement of the ureter which might lead to structuring of the lumen and hydroureteronephrosis.
This investigation further extends into several spaces. An all encompassing MRI for DIE should be done in the following list of regions, looking carefully for signs of nodules in all organs within each of these spaces
Anterior compartment
Middle compartment
Posterior compartment
Vesico-Uterine Fold
Recto-cervical Space
Uterine-Serosal Surface
Recto-Vaginal Septum
Torus Uterinus
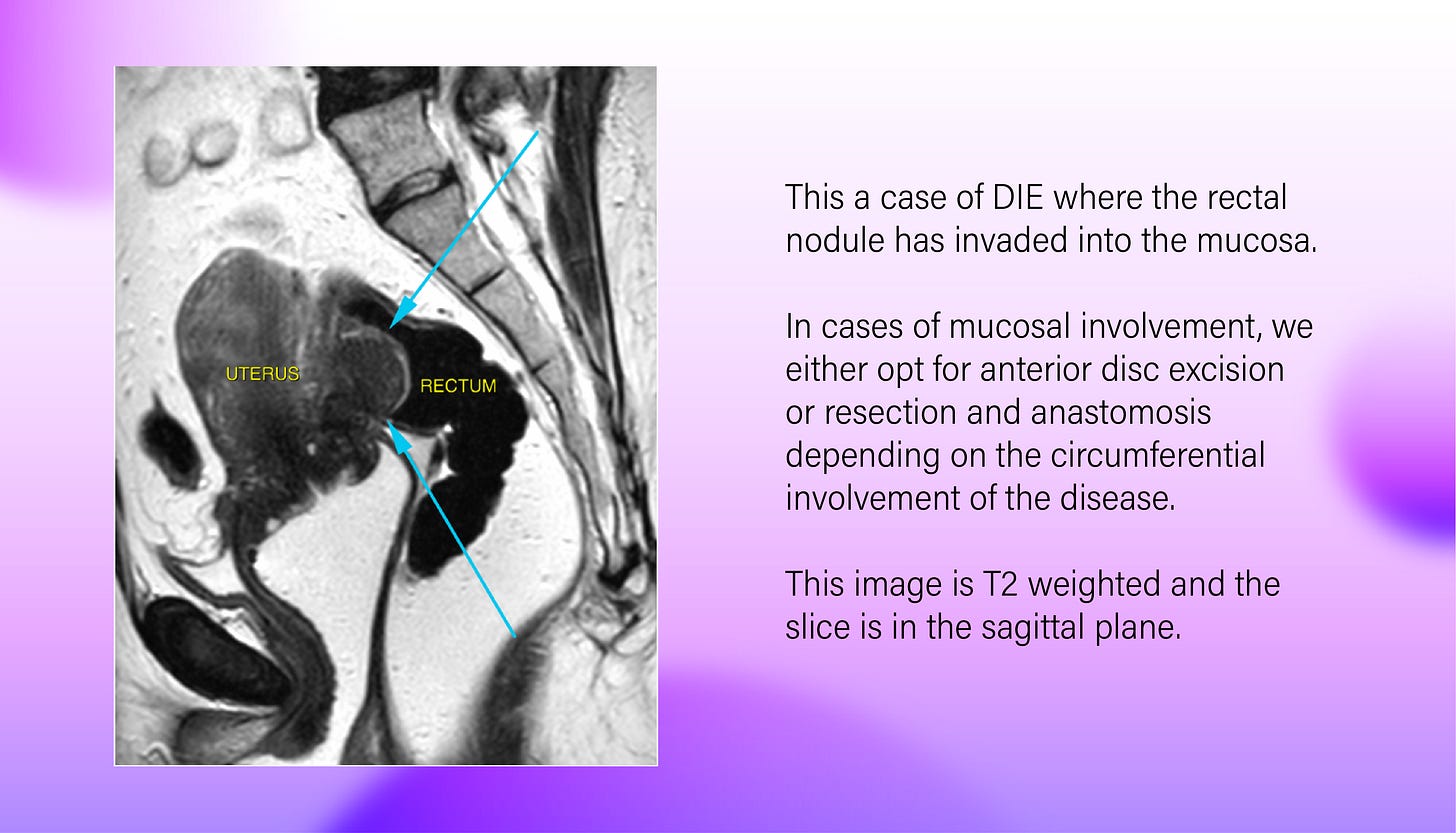
Rectal involvement, observed in the posterior compartment, in the recto-cervical, and along the recto-vaginal septum has been of much interest to doctors lately after a rise in cases of rectal involvement spurred up several different, often conflicting surgical routes.
Mayflower’s Rule of M is a framework that we use to decide our surgical plan for a case of rectal involvement in DIE and MRIs are the key images we use to implement the framework and prepare our surgical plan
More specifically, in DIE, rectum and the sigmoid colon account for nearly 90% of all cases of bowel endometriosis while the terminal ileum is the most common spot for small bowel endometriosis.
When observing large bowel nodules, there are three aspects that we particularly look out for.
Mucosal involvement
% circumferential involvement
Distance between the nodules (when multifocal)
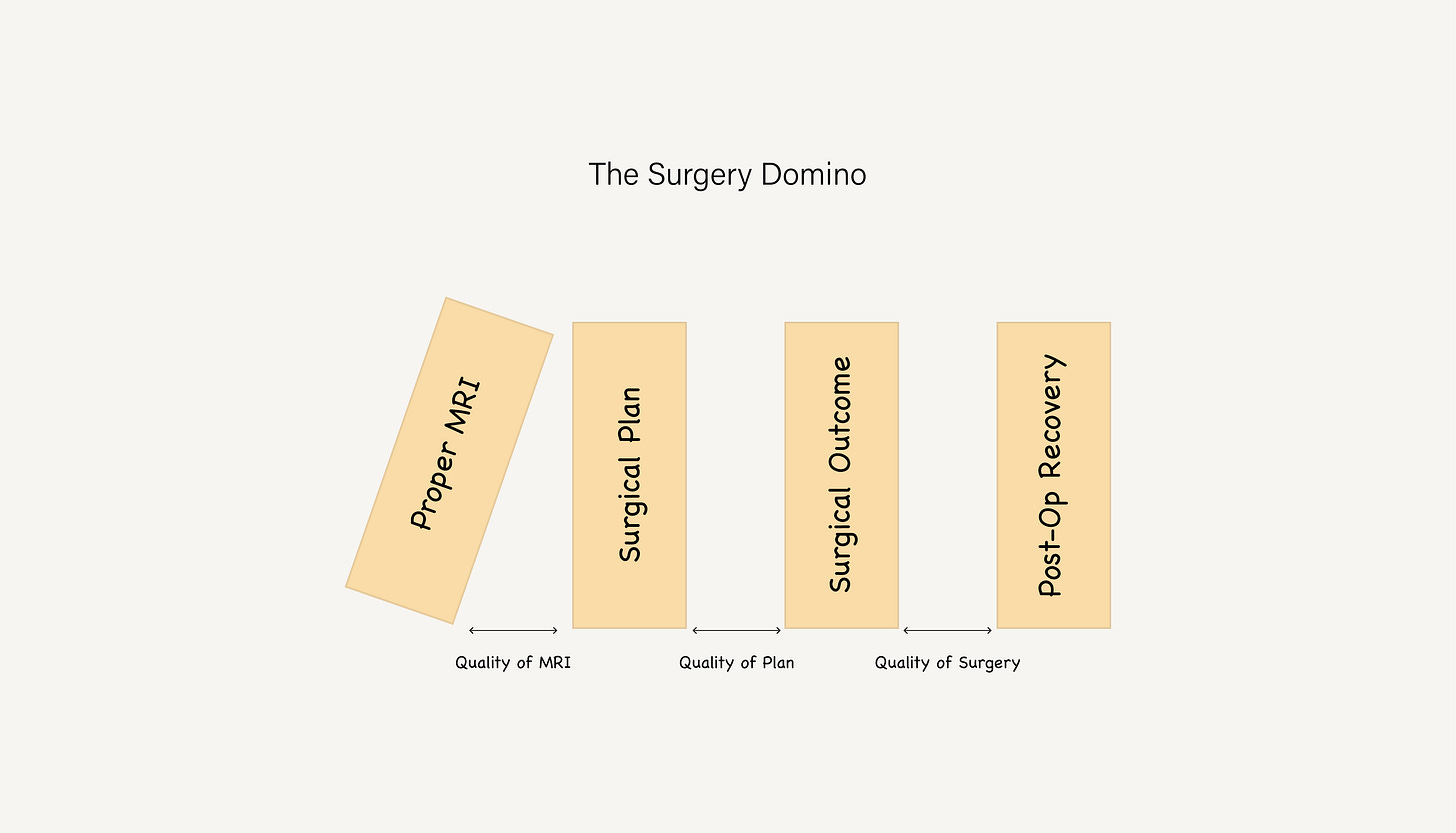
To sum it up, we’ve learnt over the last several years and thousands of patients treated, that a good surgical outcome is a product of a good surgical plan, and a good plan is the result of a good diagnosis. It’s a domino effect
That’s it. That’s the letter. If you liked what you read, please share it with a friend. If you didn’t like what you read, please share it with an enemy. Either way, help more people find out about our efforts.
Wanna join the wagon? Email us at publications@mayflowerhospital.com with your thoughts on how we can take the curation of this emailer to the next level. I will see you folks next week








Valuable Information received on MRI prerequisite for diagnosis of endometriosis Dr. Smith. Myself Dr. Kalpana Tiwari from Jaipur Rajasthan this side. Thorough this newsletter we will be benefitted dr your, and sanjay sir's vast experience in dealing endometriosis. Thank you so much for initiative.
Interesting insights into tackling this enigmatic condition