Nephrectomy in Endometriosis, and how to Avoid it
A surgery used only for the highest level of irreversible damage done by endometriosis, and how to avoid it.
It’s been another action packed week on our side. The authors for this week are coordinating across continents, with one midst a jam packed surgical week of the CSEEMIG course Mayflower, and another in a rather quaint but thoughtful city of Vienna.
Reading about the famous doctors who originated from Vienna gave us the perfect inspiration for the edition today. We want you to meet our hero for the day; Ignaz Philipp Semmelweis, also dubbed the ‘father of hand washing’. Ignaz worked as an obstetric and midwife in the Vienna university where he was the first to propose that childbed fever (rarely observed now) was actually because of the poor hygiene of doctors. Specifically an improper or no washing of hands.
This idea was met with a severe reaction from conservative doctors of the time who believed a little too arrogantly that the disease couldn’t possibly have anything to do with them. Clearly, they were wrong.
Their ignorance measured in hundered of cases of bedside sepsis. Hubris is an expensive indulgence. And in medicine, your hubris costs lives.
Things are no different in edometriosis. Parametrial involvement, that we talked about in a previous edition, can aggravate over time. Especially when left untreated, or when operated incompletely. This involvement puts pressure on the ureter leading to hydroureter first, and hydronephrosis consequently.
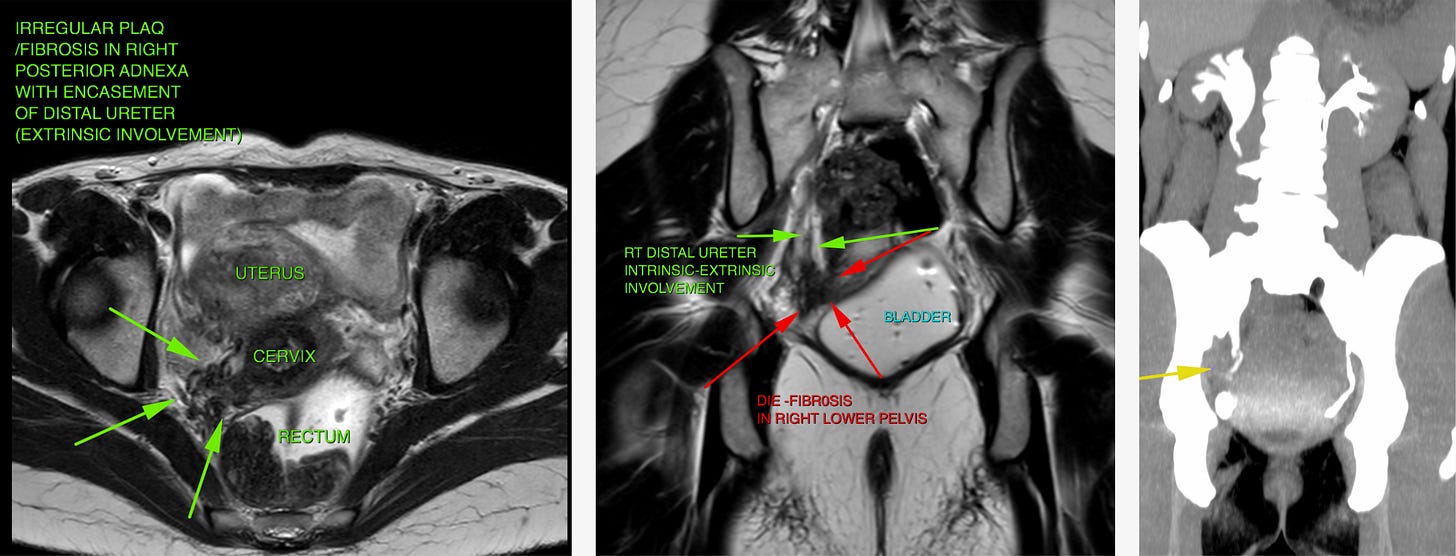
This is an MRI scan that shows both an intrinsic as well as an extrinsic involvement of the ureter and subsequent hydronephrosis. Before we ask how we operate these cases, it’s important to ask how these cases happen to be. There’s a common pattern we’ve observed in the treatment structure of patients who often reach this stage
Multiple incomplete surgeries
Single speciality (often OBGY) involvement
Incomplete counselling on disease and its impact
Objective limited to fertility enhancement
Minimal focus on pain reduction or root cause analysis
A lack of wholistic anatomy restoring surgeries
At this point, it’s almost as though the disease alone cannot be held responsible.
Parallely, a study of the physiological impact of the disease almost exclusively omits the psychological and lifestyle impact. Patients suffer years of social exclusion, personal frustration, and misguided allegations when living with the disease, furthering the already devastating impacts of the disease.
All of this suffering can be avoided if early signs of deep infiltrating endometriosis are caught, diagnosis performed completely, and the right specialists deployed for surgery along with comprehensive, and structured counselling.
In the lack of these steps, a growing disease can lead to the last level of complication in the uretric involvement of endometriosis. In an old article we called this level The Emergency Exit and the patient engagement would begin with a full MRI, and a DTPA scan.
If the results are less than 10%, we go ahead for Nephrectomy.
The surgery begins by dissecting the parametrium and performing uretrolysis. We we have dissect and free the ureters all the way from the pelvic brim down to the point of constriction and up to the kidney on both sides.
Next, we identify the intrensic nodule on the ureter and shave it off. Next, the ureter is bisected form the distal healthy part and is then used as a hammoc for traction and the dissection is carried forward in the cranial direction.
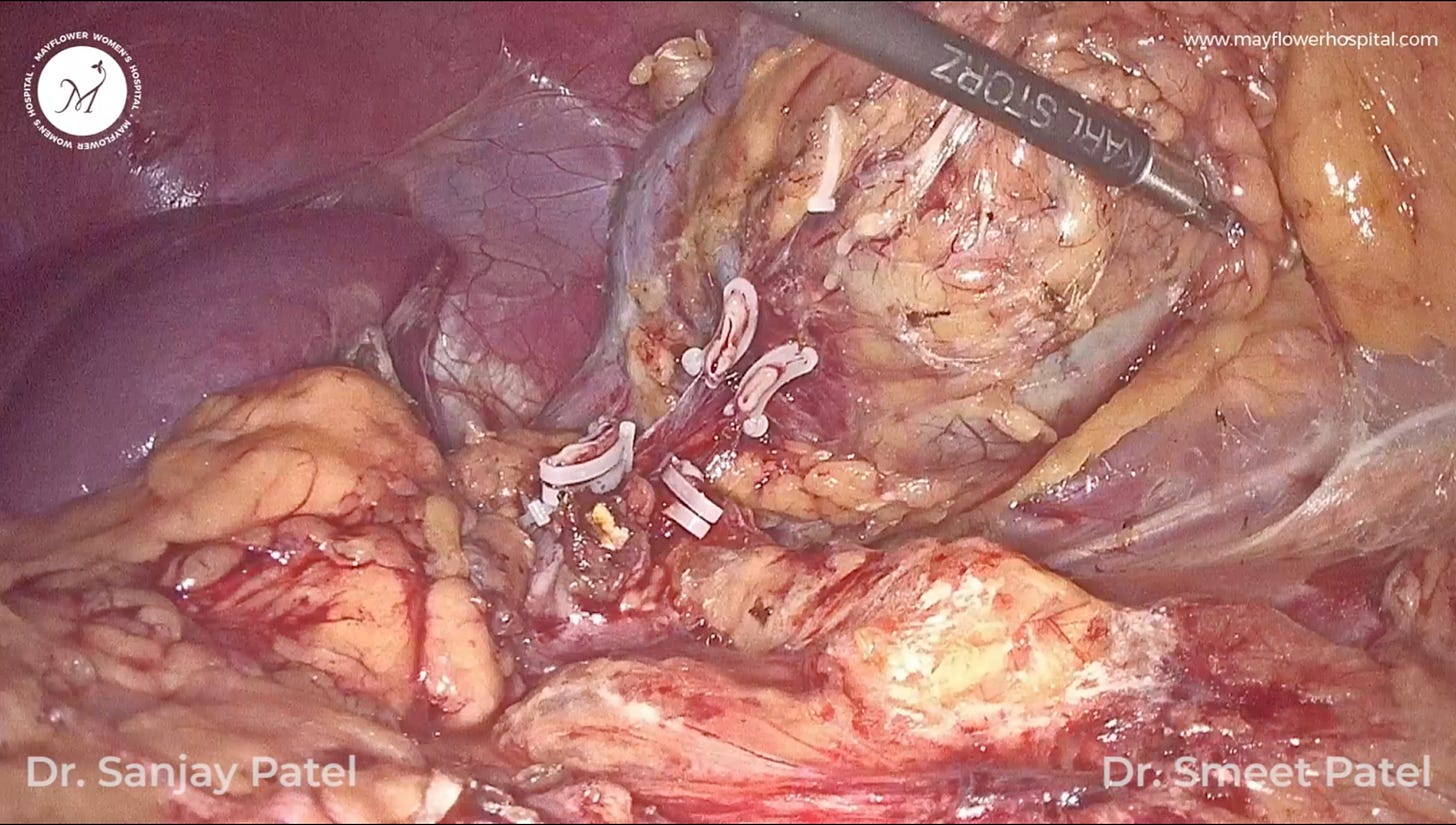
Once we arrive at the affected kidney, all the parenchymal tissue surrounding it is dissected off followed by a clipping of the renal artery and veins respectively.
One obvious yet noteworthy point is to ensure that liga clips are always placed on fresh margins. The vessel has to be skeletonised, denuded of all surrounding adhesions, parenchymal tissue and any disease involvement. While this is a general guideline, not following it strictly this particular case can leave major gaps in vessel sealing and a possible chance of burst given the high pressure within the vessel.
Moving on, the area of the pelvis belonging to the kidney is again checked for any other vascular supply. We often see a varying combination of vessels here. Two arteries, and one vein, two veins and one artery, or two arteries and veins each. Any of these cases might occur that we need to handle. Thankfully, the process of management remains the same.
A side note is that as a thumb rule 2 ligaclips are applied at the distal end of arteries, however in case of a vein, one clip is enough.
After the completion of vascular detachment, the kidney is freed 360 degree from all its parenchymal attachments and is dropped down into the pelvis.
Next, the remaining parenchymal tissue is dissected and the whole single side of the renal system is delivered outside the body.
While nephrectomy itself is a simple procedure, this involvement of the disease forces gynecologists off the comfortable seat we sit on, operating in the familiar environment of the pelvis.
We are forced to move up in the abdomen and encounter regions we don’t usually meddle with. However, our understanding of the disease, its behavior, our ability to identify the culprit tissue, and perform a total surgery help greatly in improved surgical outcomes.
Surgeries aren’t fun when they could’ve been avoided, but weren’t.
We will leave you with that food for thought today. If you have questions with surgery, or the early diagnosis of endometriotic invovlement in various systems in (and outside) the pelvis, feel free to write in to ew@mayflowerhospital.com