A few weeks back we wrote an issue titled The Unofficial Symptom Map of Endometriosis. There, we covered a broad range of symptoms and what possible pelvic co-location might lead to the symptom. One symptom in particular however has been of increasing concern.
Dyspareunia, or difficult and painful sex, commonly associated with vaginal endometriosis or plaques along the recto-vaginal fascia, has emerged as a symptom that burdens the relationships of endometriosis survivors and a imposes a heavy additional cost on their emotional well being.
So today, we double click on dyspareunia and take a hard look at ways in which it strains the lives of our patients, and the people closest to them.
“I wouldn't try because it would be like, it's going to be pain to you and the last thing I want to do is for her to be in pain.”
This quote is from the subject of a study conducted in order to understand the impact of dyspareunia in couples. This study leaves us with some interesting insights that we will discover through the course of this edition.
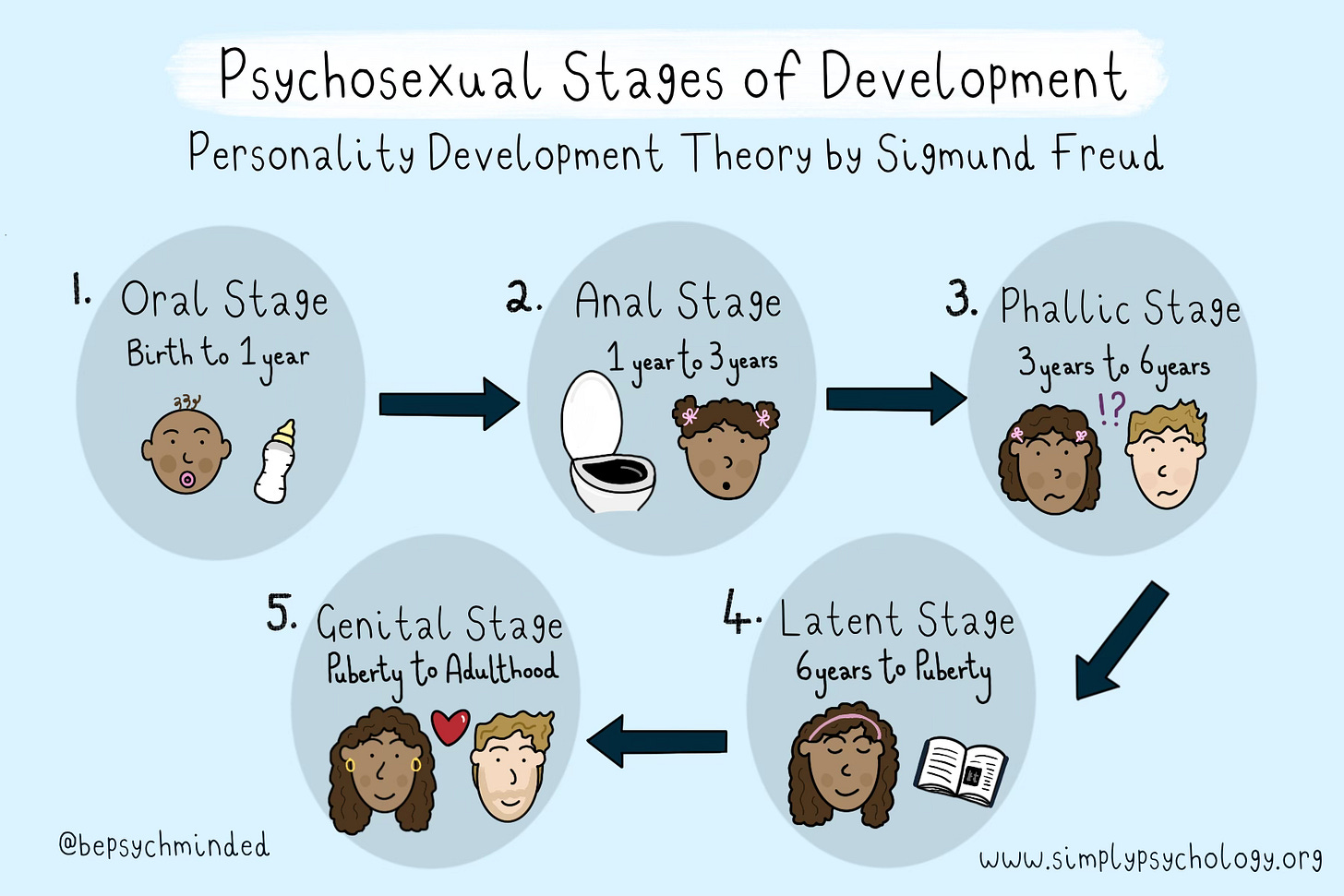
Understanding dyspareunia, or painful sex, and its impact requires us to first understand sex and what it means to us beyond physical intimacy. The impact of the absence of sex in the lives of people can only be understood once we absorb the purpose sex serves when it is present. And who better to refer to than the man of modern sex himself, Sigmund Freud.
Freud’s biggest contribution to modern medicine in general, and psychology in particular, has been the link he establishes between an individual’s self image and their sexual desires. For Freud, sex isn’t a carnal behaviour we learn once we hit puberty, or when we desire offspring. It’s instead an integral part of who we are. Ever since we are born, sex forms an essential ingredient of our growing up process. Freud described this as the psychosexual stages of development
In fact sex is so ingrained in our personality that in explaining what characterises a human personality in his ice-berg model, Freud puts the basic impulses of sex and aggression in the most hidden and core compartment of our personality, the ID.
So when the disease of Endometriosis takes over and dyspareunia drives a wedge into relationships, it isn’t surprising that this affects patients and their partners in a way that even they don’t understand. It goes beyond what they can reason with (their ego) or the beliefs they hold (their superego). It’s got a lot to do with how they are hard-wired (their id) With this lens let’s look at some profound revelations about endometriosis and relationships.
In a 2021 study on the impact of endometriosis on couples, titled “Psychological Morbidity in Endometriosis: A Couple’s Study” there has been an attempt to establish a correlation between endometriosis and the various ways in which it impacts lives.
In this paper we see that even the mere perception of endometriosis or its severity begins to impact the relationships that patients have with their partners.
(the study) showed a direct effect between perceived severity of symptoms and marital satisfaction with psychological morbidity in women with endometriosis. Studies confirm that a perception of endometriosis symptoms as severe can exacerbate anxiety and depression symptoms… Therefore, it is important to assess and help women to increase their social support in order to help decrease psychological morbidity.
A study titled “A Qualitative Study of the Impact of Endometriosis on Male Partners” published in Human Reproduction by the Oxford University Press reveals an interesting angle. Let’s look at some excerpts.
The impact of endometriosis on sex and intimacy for couples was profound. In nearly half of the couples sex was reported to be ‘non-existent’ or ‘rare’, either at the time of the interview or in a recent phase, and others reported reduced frequency of sex. Men spoke at length about the impact of endometriosis on sexual relations with their partners, though they were less likely than women to report a significant loss of intimacy, closeness and affection. The impact on sex was not solely related to dyspareunia, but also to women experiencing general fatigue, reduced sexual desire as a result of medication, low mood, the stress of trying to get pregnant, bleeding during and/or after sex, and women feeling generally unattractive and unfeminine.
“I'd be a pretty shit husband if I was like ‘well this is rubbish isn't it’ … you've just got to take it on the chin really … if it's my needs or whatever, who gives a toss about that, let's, like I said, get her better. It's not about me.”
Most men understood why it wasn’t possible, and what the right thing to do was, but it was still done under a recognition of the loss of an important aspect of their intimacy. Sex wasn’t crucial but they weren’t indifferent towards it either.
On having children, one account in particular stands out, and echos several such similar feelings we’ve come across during counselling
“Coming to terms with not having children of our own and the whole process of IVF, going through it, is really traumatic and for me that's been the most painful element of the whole process … I have never gone through the kind of extended period of profound misery and disappointment as I have with IVF.”
Low frequency of sexual activity and sexual dissatisfaction in patients with dyspareunia, due to the presence of pain and difficulties during sexual intercourse, have been associated with higher psychological morbidity in women - the study quotes
Dyspareunia is much more than a pain manifestation of ectopic tissue growth. It’s the disease attacking on our deepest perceptions and fundamentally altering how we see ourselves, and in turn, the people who love us.
As doctors, we must focus on how we can understand this aspect of our patient’s lives better, help them have a candid conversation about it, and in the course of treating the disease, perform a surgery that helps restore their anatomy and help lead a disease free life.
That’s it from us this week. We would like to send a special thanks to Himani Dhandhukiya for helping us better understand the works of Sigmund Freud and its relevance with our battle against dyspareunia.
Footnote: If you have recurrent pain during sex, talk with your healthcare professional. Treating the problem can help your sex life, your emotional intimacy and your self-image.