Juhi Never Thought That Life Was Gonna Be This Way
Imagine you’re a woman in your 30s. Your second child has just started going to school, you’re beginning to find your old self back, planning your career ahead, applying for jobs, giving interviews when you start to realise that your periods have gotten worse over the last few months.
More painful, greater blood flow, sharper mood swings.
You think it’s the age. That’s what everyone tells you. Mid 30s can be difficult.
But then slowly, you start experiencing pain during sex. Love making isn’t fun anymore. Relationships start to strain.
Frustrated you begin to see doctors and before long, words like fibroids, adenomyosis, and endometriosis enter your vocabulary.
You’re now in denial. You change from one doctor to another, you think all this is being done to put you into some surgery trap.
You just want to get back to your life. You agree with whoever tells you medicines can help.
You do that. But it doesn’t help.
You’re now angry. You start discovering more women around you who’ve had this condition.
And you start hunting for hope. Maybe there’s a better, easy way out. Surely someone on the internet would’ve figured it out. You’re now bargaining.
All this while, your symptoms haven’t gotten any better. The medicines are suppressants but they don’t cure anything.
The pain got better but a lot else is getting worse. You’re about to find out.
2 years have passed. The medicines have hit a plateau. There’s only so much they can do and the symptoms have now started coming back.
Your life is haywire. You keep cancelling social meets, you haven’t gotten back to work in ages. Life is slipping away from the middle of your fingers the tighter you try to grip it, like trying to hold on to sand.
Depression kicks in. Everything feels meaningless, all the doctors feel like they’re just trying to sound smart but they know nothing.
No one understands your pain. However hard your family tries to help you, you’re convinced they simply can’t.
You don’t even remember the person you once used to be. Your kids are growing up and growing apart from you and that’s a whole different emotional roller coaster.
You’ve hit rock bottom. The only way from here is up. You reach acceptance. You’ve had enough and you start seeing experts who will give it to you straight. This is exactly where our story begins today.
Juhi (name changed) came to us after several years of improper diagnosis and blind medical management. She got referred through a very well known uro-surgeon of the country, and for the first time, after having fought and lived with the disease for more than 7 years, did someone choose to send her for an MRI.
For the first time, you see the truth.
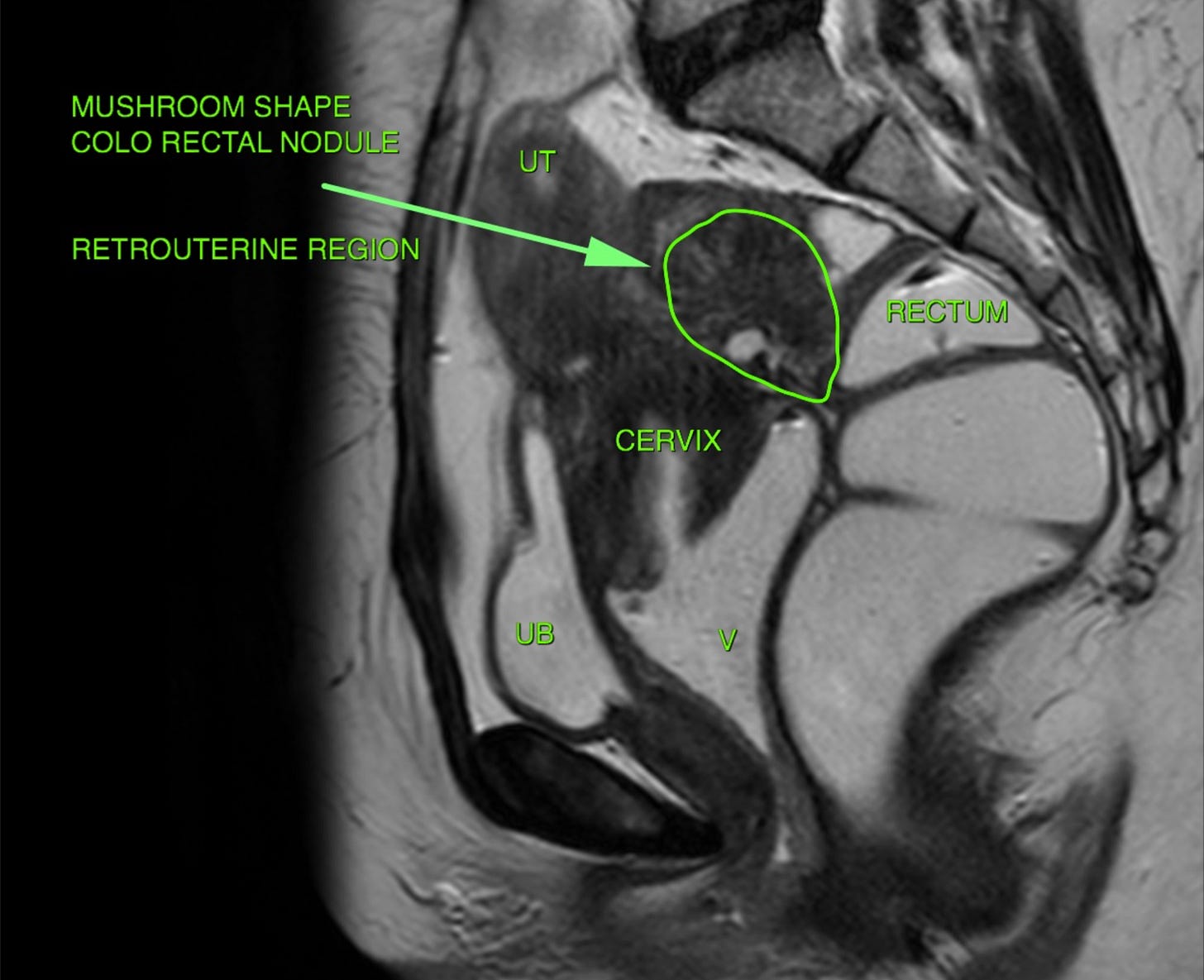
There’s a large colorectal nodule, the torus-uterinus is involved, and the ovaries are adherent. The uterus is adenomyotic and the muddy nucleation on the MRI suggests that years of medication has made the endometriosis tissue rubbery, rigid, and hard to dissect.
There’s a typical mushroom shaped nodule in the colo-rectal region. With the retro-uterine and recto-vaginal aspects involved, you finally get to see what’s making sex so difficult for you.
As a bystander this diagnosis can feel harrowing. You feel bad for the person. But from the hundreds of sessions of counseling I’ve done, I can assure you that a misdiagnosed and mistreated patient finds this reliving. Finally, they can see the enemy for what it is.
Now step out of the Juhi’s shoes. And step into mine. Because the mindset need to treat a case like this is a whole lot different.
The Surgeon Takes Charge
Remember, in surgery, “Cut Follows Cause” always. What you do must be driven by a purpose that serves the patient, and the betterment of their life. Surgical decisions should always rest upon those principles and derive themselves from those purposes.
In this case, we were very clear from the get go that Juhi deserved
A permanently better quality of life, which can only be achieved through
A complete removal of the disease
A neat and clear surgery
Anatomical restoration
A claim over her old self and the ability to feel normal again
Just how the opposite of patriarchy is equality and not matriarchy, the opposing force to an aggressive disease must be thoughtful, careful, and purposeful surgery.
We deal with the tissues with love and care. Being mindful of what to retain, and what to let go. Best way to do this is to not push or pull, but to identify the right plane, create the traction we need, and dissect with passion.
Restoring the Anatomy
Restoration begins all the way at the beginning of the surgery itself. we identify the organs, and try to normalise the anatomy with clear cut dissections in the right plane.
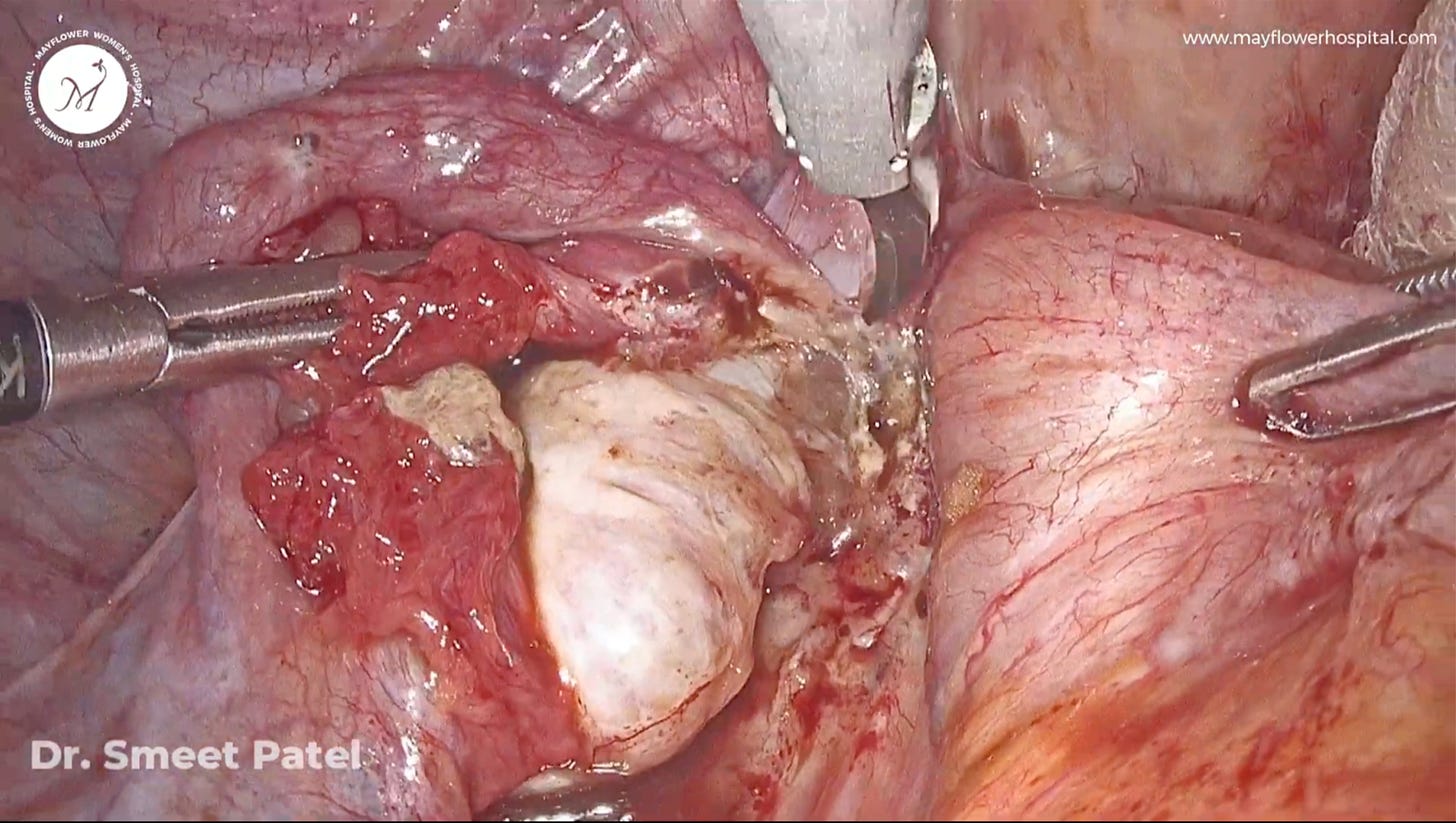
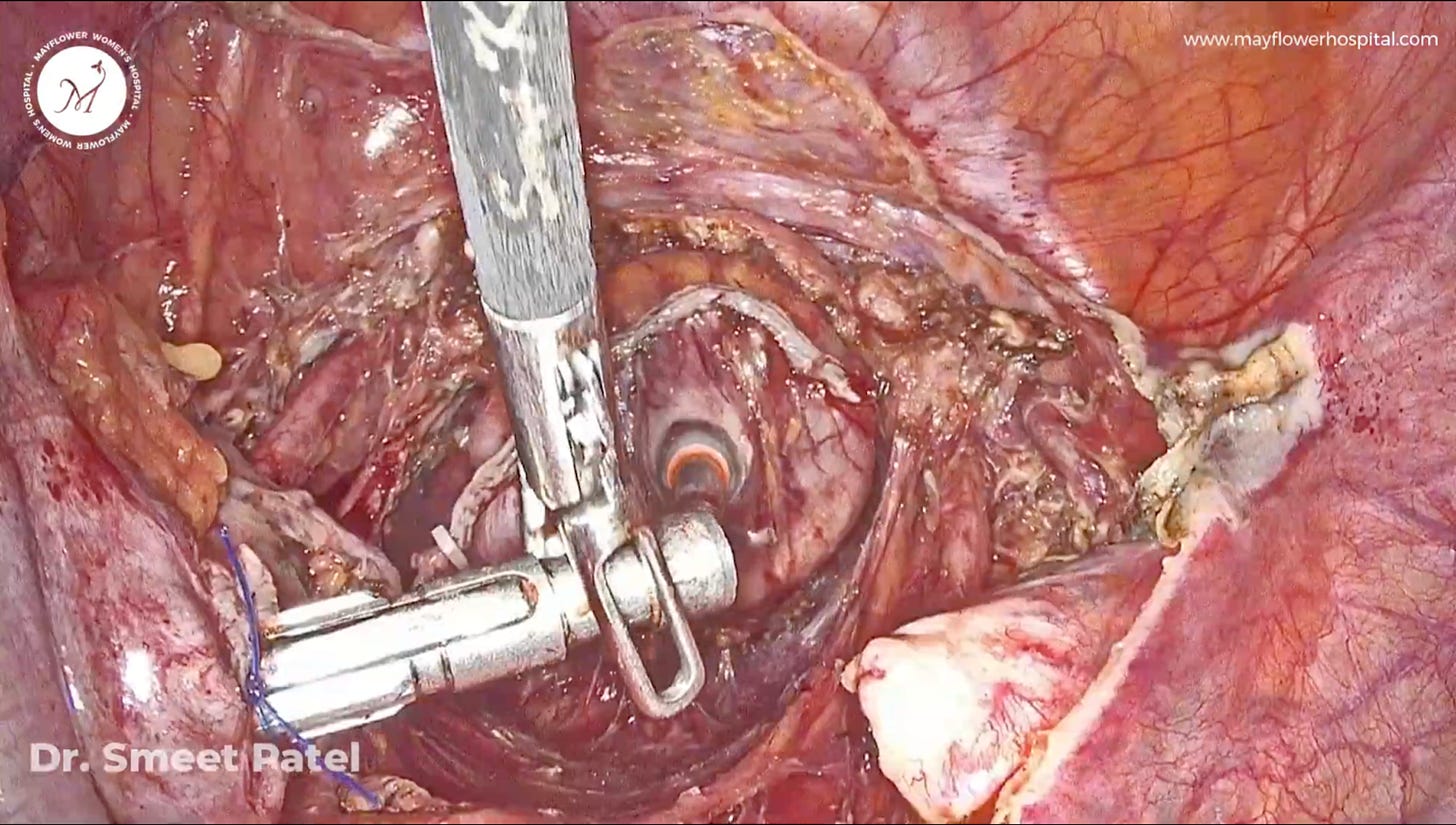
You can see our dissection over the ovary in the image above. The most important step here is the identification of the ovary and its dissection away from all the adhesions and endometriotic nodules surrounding it.
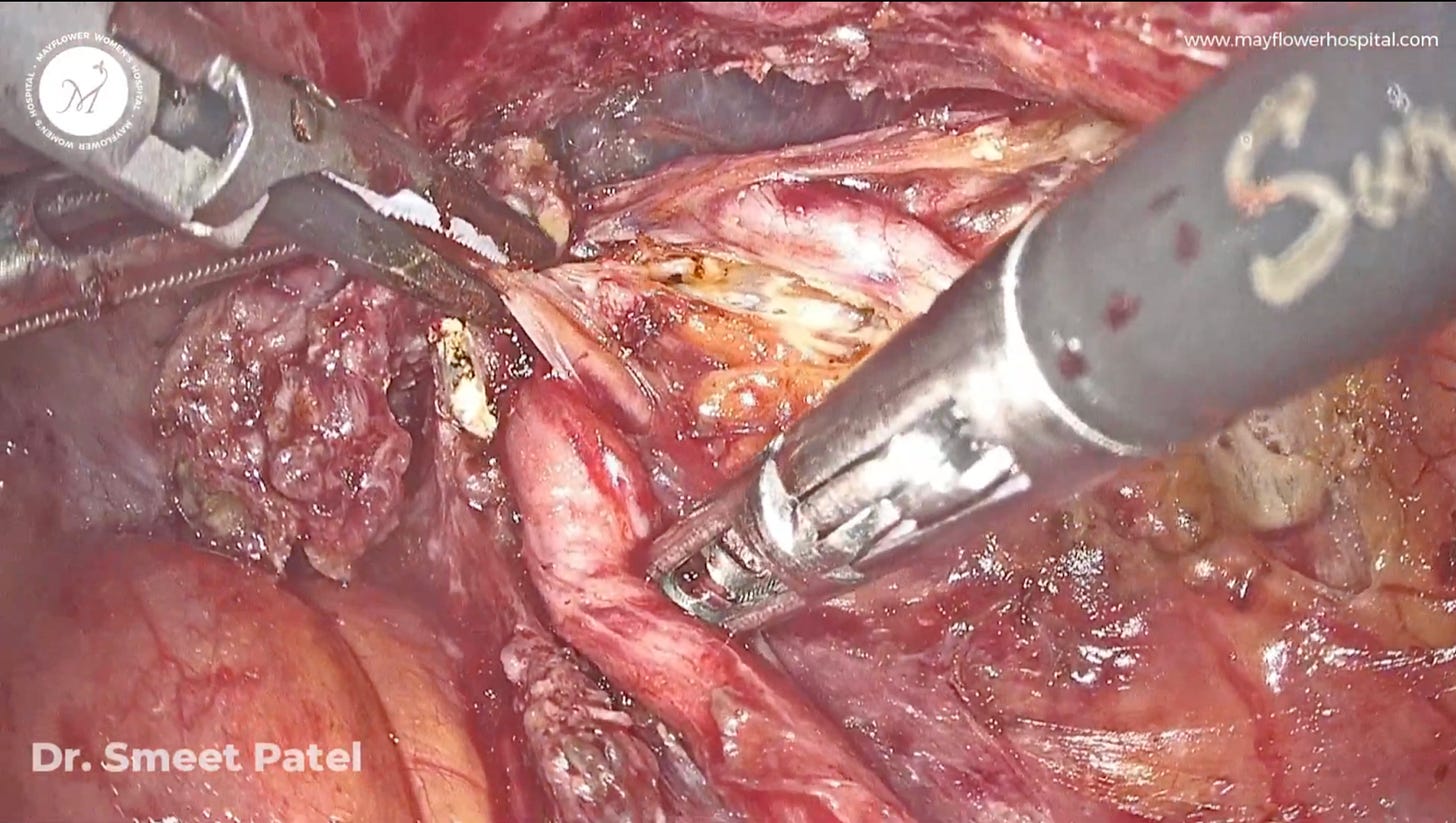
Once we’ve freed the colon, and the ovaries, we proceed to uretrolysis
As a first step, the ureter is identified at the pelvic brim, a nick is made on the anterior peritoneal reflection, creating a cleave in the tissue. This cleave must be propagate parallel to the ureter and that’s precisely why giving traction normally to the ureter is crucial.
Improper traction will build an improper plane, and the line of dissection will start going on a road trip of its own.
Ureterolysis is conducted caudally all the way till the Tunnel of Wertheim.
We go slowly, fibre by fibre, so as to always be conscious about the traction line and the dissection’s direction relative to the underlying ureter. As we proceed and the tunnel of Werthiem, we remove all nodules present on the ureter.
In this case vascular webb dissection is done, after which the uterine artery is identified and clipped.
All the parametrial nodules over the uterine vasculature are identified, and dissected with the procedure continuing all the way upto the tunnel of Werthiem.
This is where we perform the de-roofing of the tunnel - that’s right — we remove all the nodules over the anterior surface of tunnel. It’s a bit of a tricky pose but with time and practice, you manage.
We remove the plaque surrounding the ureter, uterine artery and the notorious venus plexus - without injuring any of the surrounding structures, and most importantly in a neat and clean way.
Pro Tip: For fine dissections use only the tip of the harmonic and move the probe away from the organ to get a clean dissection line without injuring any of the underlying structures
Now we move towards the medial pararectal space dissection.
We identify the correct plane and dissect parallel to the rectum.
The hypogastric nerve must always be preserved. A nerve sparring surgery gives great post operative recovery and saves the patient some precious visits to the doctor and a lot of bother. Similar steps are done on the opposite side as well.
Remember how I showed you that the patient’s endometriosis tissues would be in a bad state. This is where it gets tricky.
As a side effect of medication the tissue goes from being laminar to thick amorphous and rubbery. Because of that we face great difficulty in finding the planes easily and the surrounding tissue in a state of affair where there’s no legitimate traction and counter traction available.
The tissue is dense and rubbery in consistency. The dissections suffer, but somehow we manage. At times like these I often wonder if the tool is slow or if I’m too fast.
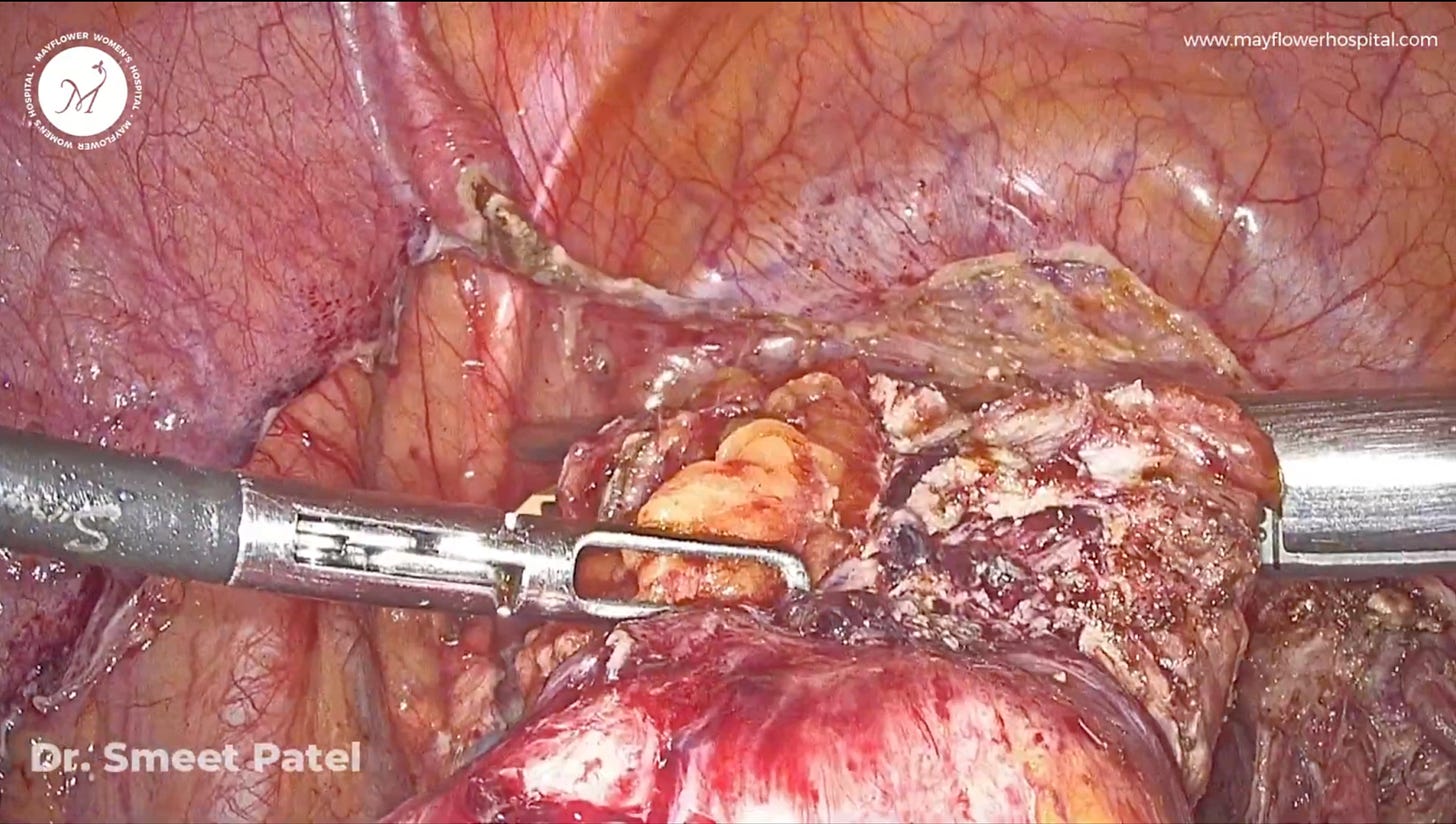
Next, we remove all the peritoneal involvement to finally expose the colonic involvement and considering the factors listed in Mayflower’s Rule of M, a decision is taken to perform resection and anastomosis.
We are generally very conservative in our approach but the disease demands R&A owing to the involvement.
We enter into the holy plane; go deep down and dissect off all the parenchymal tissues along with the endometriosis nodule.
Tracing the dissected medial pararectal space and holy plane, at the centre of the caudal region we have the lower end of the rectum, vagina and a part of the cervix : all jammed up with a recto-cervico-vaginal nodule.
Here we have taken an approach where we follow the holy plane and come caudally, and eventually reach the anterior aspect of rectum. Here we dissect in a layer by layer approach - like cutting through lasagna, and we eat each layer separately and enjoy it. (not literally of course)
Making the colon completely mobile, we move to denuding the fat. A clean surface is essential in ensuring a complete R&A procedure. The use of an advanced bipolar device is preferred here.
Just distal to the rectal involvement we take all the fat surrounding the nodule from around the affected colo-rectal region’s perimeter - we make the rectum naked of fat.
This is where we apply a linear stapler.
Next, a TLH is carried out, and the uterus delivered outside through the vagina.
Now we need mobility of the colon for a tension free anstomosis.
We start from the sacral promontory, dissect the peritoneal reflections and the parenchymal tissue surrounding the inferior mesentric vessels. They are skeletonised and clips are applied and a cut is placed. Thereby giving us a mobile colon.
After achieving this, the colon is inspected, a linear stapler is inserted, position taken and boom! shots fired
The transected colon is delivered out through the vagina (natural orifice surgery).
The diseased part of the colon is removed, an anvil is inserted and purse-string sutures are taken surrounding it.
The colon with the anvil is delivered back into the abdomen, a circular stapler is inserted from the rectal orifice and advanced.
The anvil is locked into the shaft of the stapler and the stapler is closed.
One point to note is that there is healthy parenchymal tissue on both the ends which is why the circular stapler is compressed to the green limit and only then finally fired.
Next, the vault is closed, surgical site introspected, and once all is neat, clean and good to go, the port sutures are taken.
The uterus was removed, but importantly, the ovaries were preserved. The patient, keen on and benefiting from the organ’s cardioprotective hormones, was relieved to retain her ovarian function.
Closing meticulously, we placed what we hoped to be the patient's last stitch ever for endometriosis.
That’s it for this week. A bit long, but we think worth it. See you next Wednesday.