How to measure surgeons without triggering their egos
You're doing it wrong and you need to fix it
It’s Ganesh Chaturthi here in India today. Celebrated most fervently in central parts of the country, it’s a festival that has permeated societies and chances are you might see a Ganpati pandal even if you’re somewhere close to Indians today.
So Happy Ganpati! to whoever is celebrating! If you’re reading this from anywhere near a Ganpati shrine, please send us pictures! We will share them in the next edition!
Here are the ones from our homes
Alright. On that bright note, let’s move on to today’s very important edition.
I’m sure you remember that story where Shiva and Parvati ran a grand race between their two kids, Ganesh and Kartikey to determine who gets to keep a certain divine fruit.
Rules of the game were simple.
Whoever can run around the world thrice the fastest, wins.
For those of you not familiar with the story, here’s a super abridged version. Lord Ganesh wasn’t particularly known to be athletic. To make matters worse, his vehicle was a mouse, not known for its speed. Lord Kartikey on the other hand rides a nifty peacock that can fly, and is arguably must faster. Faster than a mouse for sure.

“Easy win” Kartikey must’ve thought to himself and bolted. Ganesh on the other hand took a moment, thought, and then ran around his parents Shiv and Parvati thrice. “You’re my entire world” he said.
The result? Ganesh won.
It’s a beautiful and adorable story, but if the divine fruit was really important, you and I can both agree that there could’ve been a better way to evaluate the two kids.
At the outset, the exam itself was unfair. And in the end, Ganesh won simply on technicality. Neither is desirable.
We’ve all been in the face of unfair tests. Sometimes we’ve lost to technicality, sometimes we have been handed an unfair starting condition. And on some other occasions, we have been the ones setting the rules. Today’s edition is all about that last bit.
Sooner or later in private practice, the day arrives.
Your clinic grows. The waiting list lengthens. You bring in a junior, maybe two. Suddenly, it’s no longer just you.
The entire year passes by and the day comes for salary revision. The day you ask yourself a tough question, “which one of them did better?”
Welcome, to the most lightly handled but managerially critical point of your professional journey as a leader. How you choose to evaluate these juniors will make or break the future of your practice. It will set cultural standards and define if you will still be scribbling prescriptions or living your dream life 10 years from now.
“Wow dude calm down what the heck?” You must be thinking. By the end of this edition, it will be abundantly clear to you why answering this question is such a big deal. But for now, let’s make some assumptions.
Most doctors pick a single yardstick.
Some use patient satisfaction — “patients like Dr. X more, so she must be better.”
Others look at complication rates — “Dr. Y had none this month, clearly he’s the safer pair of hands.”
A few even measure OT speed — “Dr. Z finishes fast, so she’s efficient.”
Each of these feels neat. Each is also a trap.
A smiling patient doesn’t guarantee no recurrence.
A quick surgery may mean corners cut. Lesions left behind.
A complication-free month may mean juniors never touched the instruments.
The problem isn’t the surgeon. The problem is the scorecard.
One metric will always distort behavior. Moreover, most metrics become victims of the Goodhart’s Law.
When a measure becomes a target, it ceases to be a good measure
When surgeons know they are being measured for one thing, they start to optimise for just that. It’s precisely why corporate hospitals, that often optimise for revenue, have generally poor patient satisfaction scores, even after getting some of the best doctors available for hire.
Surgeons, like all professionals, perform to what they’re measured against. If you only reward patient smiles, expect theatrics in the OPD. If you only reward speed, expect reckless shortcuts in the OT.
Every metric has a blind spot. Used alone, it doesn’t measure performance — it distorts it.
That’s why the Balanced Scorecard matters. It gives surgeons four different mirrors instead of one. Not just how fast or how safe or how liked — but how balanced.
“Oh no! What do you do now?” — Don’t worry. I’ve found something for you.
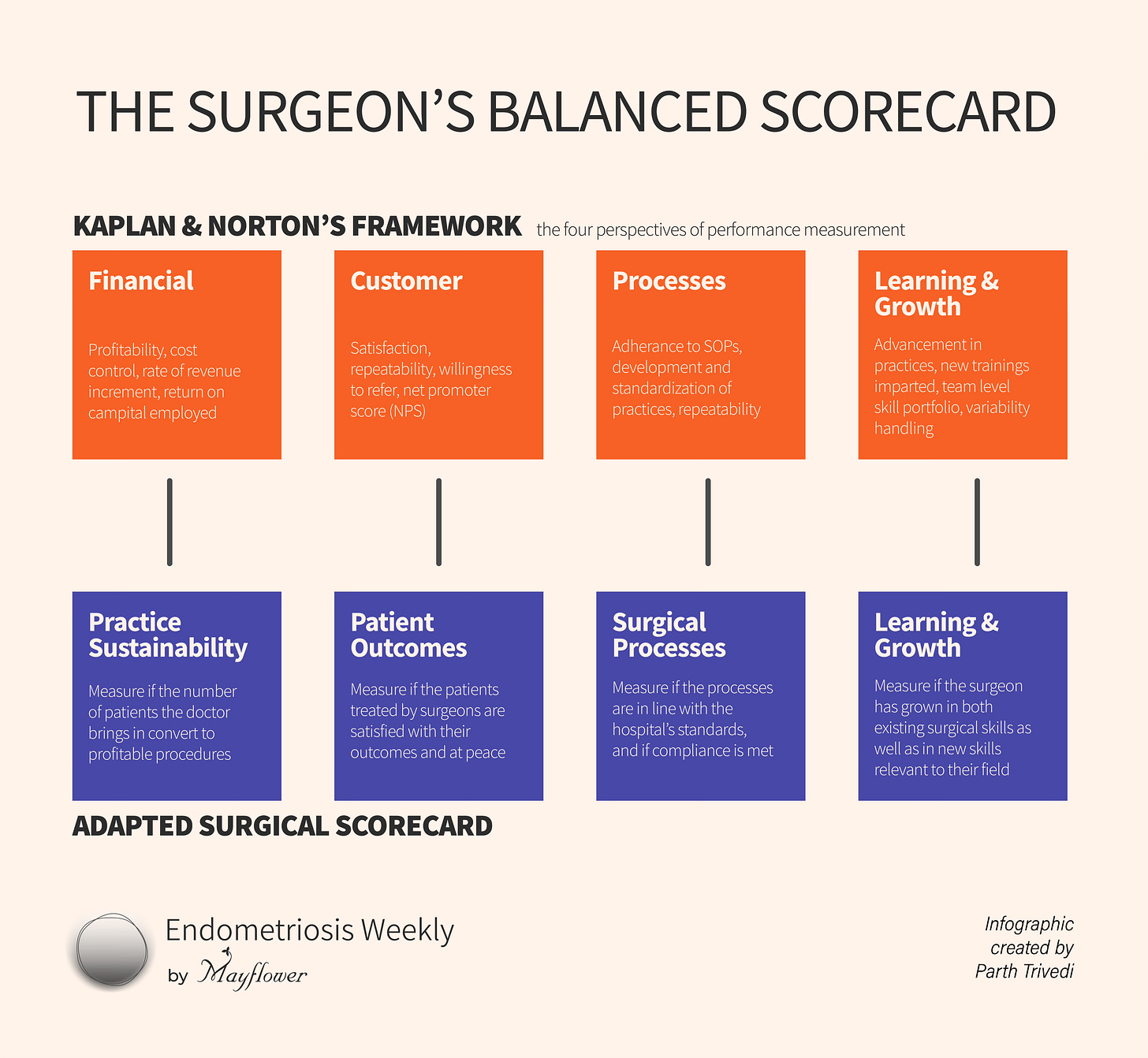
Kaplan & Norton wrote an article in 1992 titled the Balanced Scorecard what became one of the most cited business articles of all time. Instead of one metric, they proposed four perspectives of measurement. A holistic way to see performance without distorting it.
Their argument was simple, almost obvious in hindsight:
if you measure performance only by financial results, you’ll warp the business.
A company obsessed only with quarterly profit will underspend on R&D, mistreat its customers, and burn out its people. It may look “successful” this year — but the foundations rot.
Kaplan & Norton suggested four complementary perspectives instead:
Financial — are we viable?
Customer — do we delight those we serve?
Internal Processes — how good are we at the work itself?
Learning & Growth — are we building the capacity to keep improving?
The genius wasn’t the categories themselves. It was the balance.
No single perspective tells the truth; all four together do.
Now swap “business” for “surgery.”
If you judge only by patient satisfaction, you reward charisma.
If you judge only by complication rates, you reward avoidance.
If you judge only by OT speed, you reward shortcuts.
Surgeons, like businesses, need balance.
Let’s dive deeper into what these mean
Practice Sustainability (Financial / Strategic Perspective)
A brilliant surgery that no patient can afford is not brilliance — it’s vanity. Sustainability means using OT time efficiently, keeping costs realistic, and ensuring patients can keep coming back. It also means referrals, reputation, and continuity.Patient Outcomes (Customer Perspective)
At the end of the day, this is why we operate. Did the patient’s pain improve? Did fertility return? Was recurrence avoided? But outcomes go beyond the scalpel: was counselling clear, was trust built, did the patient feel heard? A disease-free pelvis means little if the patient walks away confused or alienated.Surgical Processes (Internal Perspective)
Every surgeon knows how matters as much as what. Did the excision respect nerves? Was the ureter traced properly? Were planes maintained? Was the OT run with discipline, or did chaos rule? Internal processes are the invisible backbone of good outcomes.Learning & Growth (Future Perspective)
Surgery is not a solo sport. Are juniors getting their hands on instruments? Is the senior still learning new techniques? Does the team show up for peer review? A practice that doesn’t invest in learning will collapse under the weight of one superstar.
Taken together, these four quadrants offer a fairer, fuller, and frankly more honest way to judge surgical performance.
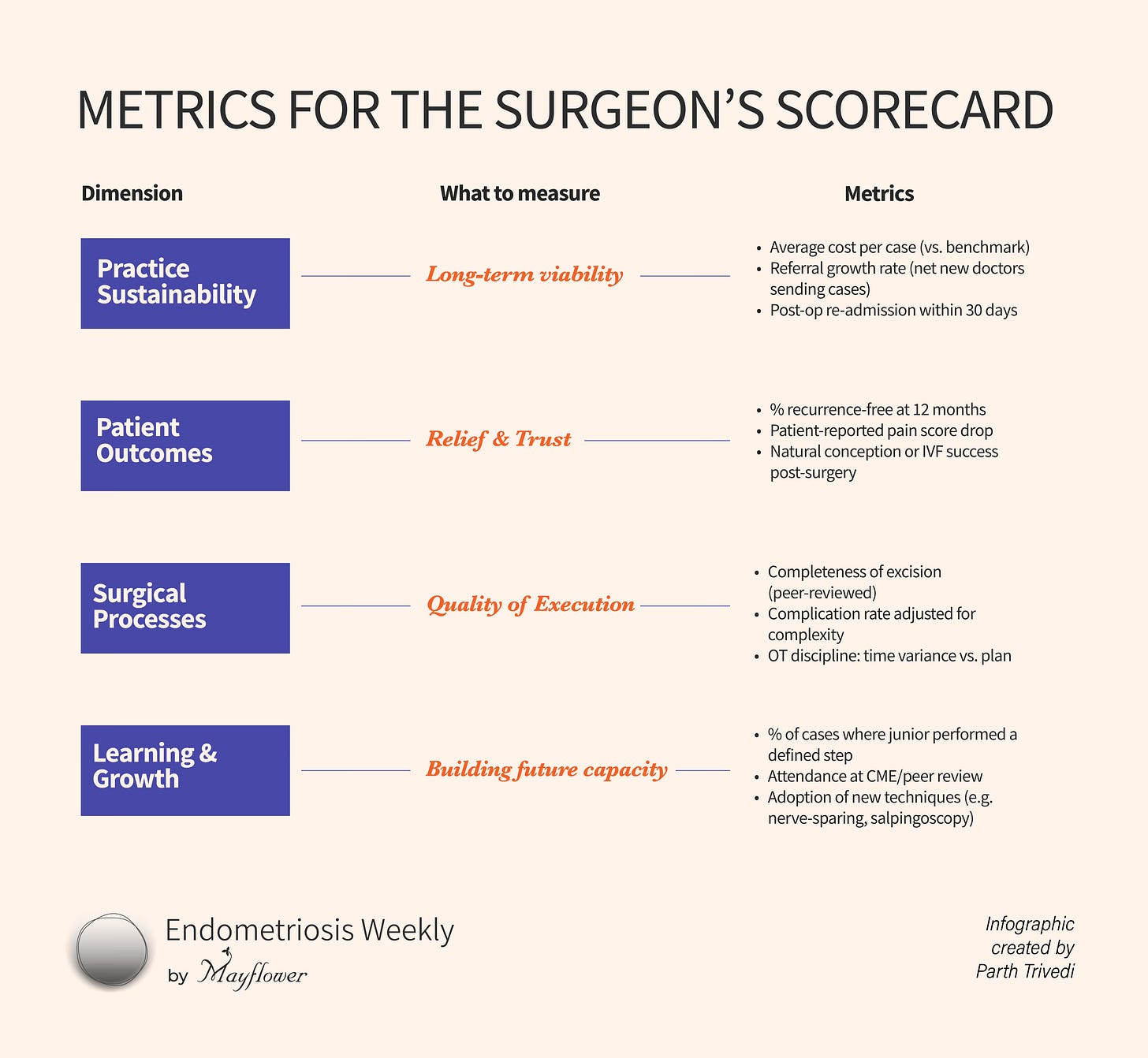
Next, we must decide what we want to measure. These are just areas. Now we will decide on the metrics. The actual measurement.
I know for a fact that doctors aren’t used to data keeping. It doesn’t come as intuitively, feels tiring, and its use isn’t intuitive. But I promise you, this next part is all a function of the data you keep and how detailed it is.
This is not about turning surgery into a spreadsheet. It’s about fairness.
A junior who takes extra time but teaches a resident is not “worse” than a senior who finishes fast but hoards cases. A surgeon who earns patient trust but ignores peer review is not the full package either.
When you look across all four quadrants, you start to see the whole surgeon. Not just who cut fastest or who smiled the most, but who is building a practice that lasts.
I know what you’re thinking right now. “Yeah yeah all this looks fancy on paper but have you ever tried actually evaluating a surgeon?” My answer is yes. I have. And I have burnt my fingers doing it. Which is why I don’t make my advice lightly.
The Reality Check: Ego and Resistance
Every surgeon carries an ego into the OT, and often outside it. You need it — confidence is what steadies the hand. But the same ego that saves you mid-dissection will fight you the moment someone tries to measure you.
Ask a surgeon to be rated on patient smiles, and they’ll say, “I’m not here to win popularity contests.”
Judge them only on OT speed, and they’ll fire back, “This isn’t Formula 1.”
Point to complication rates, and they’ll mutter, “Try doing the cases I take on.”
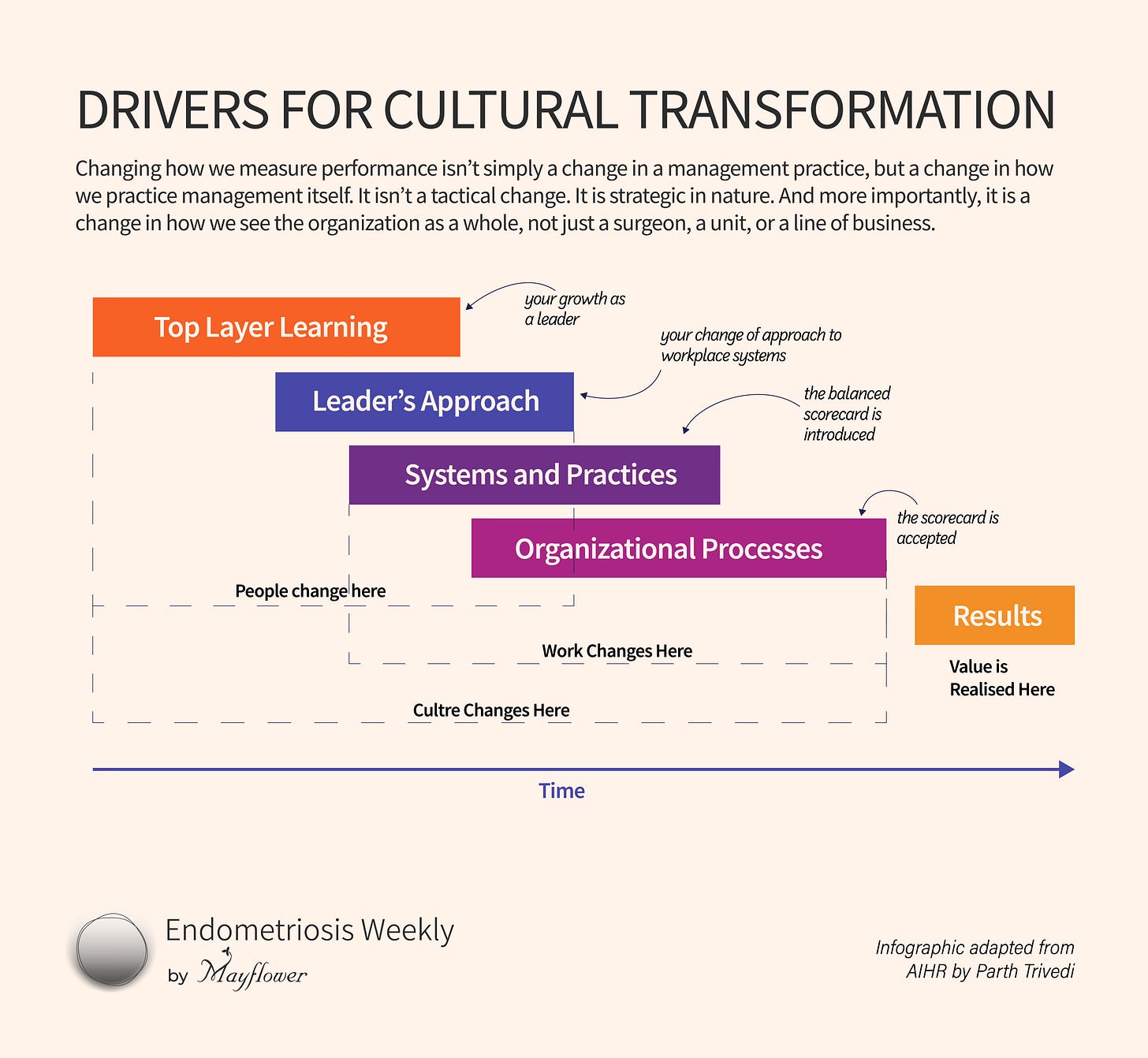
Resistance isn’t laziness. It’s pride. Surgeons see measurement as an attack on identity.
As a leader, the hard job you must do isn’t making the right balanced scorecard, but convincing your team that it’s a good thing. That it’s made to measure and recognise their strongest traits while helping them grow where they need it the most.
This doesn’t happen overnight. Sure, you can force a new method on to people. You’re the boss. But it won’t last. Even worse, it will and it won’t work. Implementing the balanced scorecard is a matter of strategy and cultural transformation.
The biggest and most important truth about any kind of transformation: It starts at the top, it starts with YOU.
No change is sustainable, no metric good enough, if we don’t take a new lens for looking at old problems.
That’s it from us this week. Please share your thoughts in the comments below or reply to this email. We would love to hear from you!