An Easy Guide to Salpingoscopy
A classification of fallopian tube health and the associated likelihood of natural pregnancy
Tubal patency is a big deal. Fallopian tubes or the salpinx are more than just a passive conduit; they serve a critical function in conception, with sperm transport and capacitation, oocyte capture and movement, embryo harbour, and more.
The most common way of assessing tubal patency is an HSG or a hystero-salpingo-graphy where an X-ray contrast dye is injected into the uterus through the vaginal route and its permeation into the tubes observed, along with the shape of the uterine cavity.

HSG however only paints a partial picture. It informs us about cavitation, not about the functional health of the fallopian tube. To go one step further, we visualise the interior of a fallopian tube. In today’s edition of Endometriosis Weekly, we take a deep dive into the use of Salpingoscopy for grading tubal health and the likelihood of conception in each case.
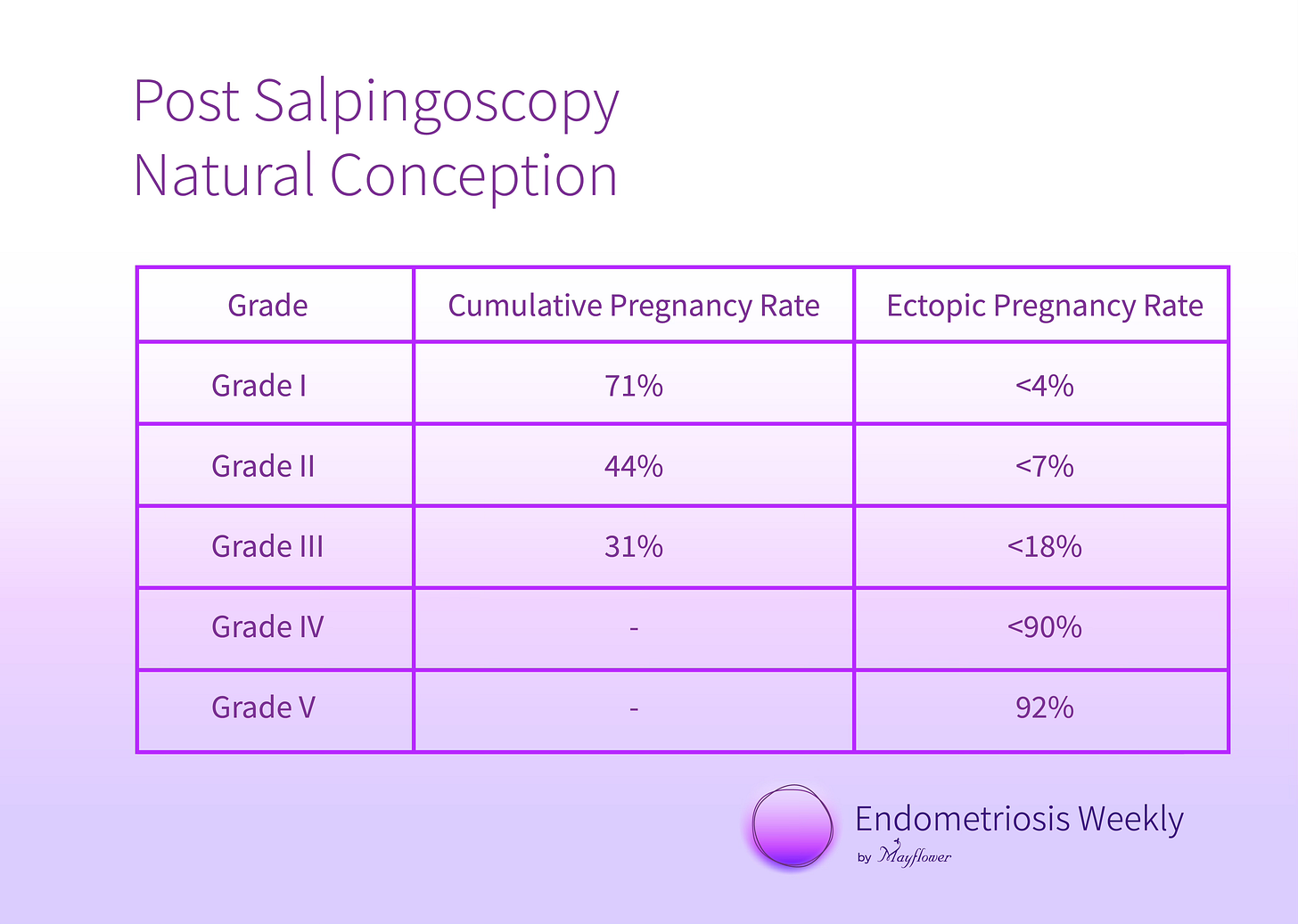
Doctors at Mayflower gauged close to 4000 patients undergoing salpingoscopy over 10 years to categorise the health of their tubes into various grades, and at the same time observe how some unique conditions like tuberculosis and hydrosalpinx may be handled.
Owing to the delicate nature of the tube and the fine cilium that lines its inside, the only way to visualise is to stick a camera into the space and take a good look. Because of its several advantages, laparoscopy becomes the ideal method for measuring tubal patency and permeability in cases of unexplained infertility.
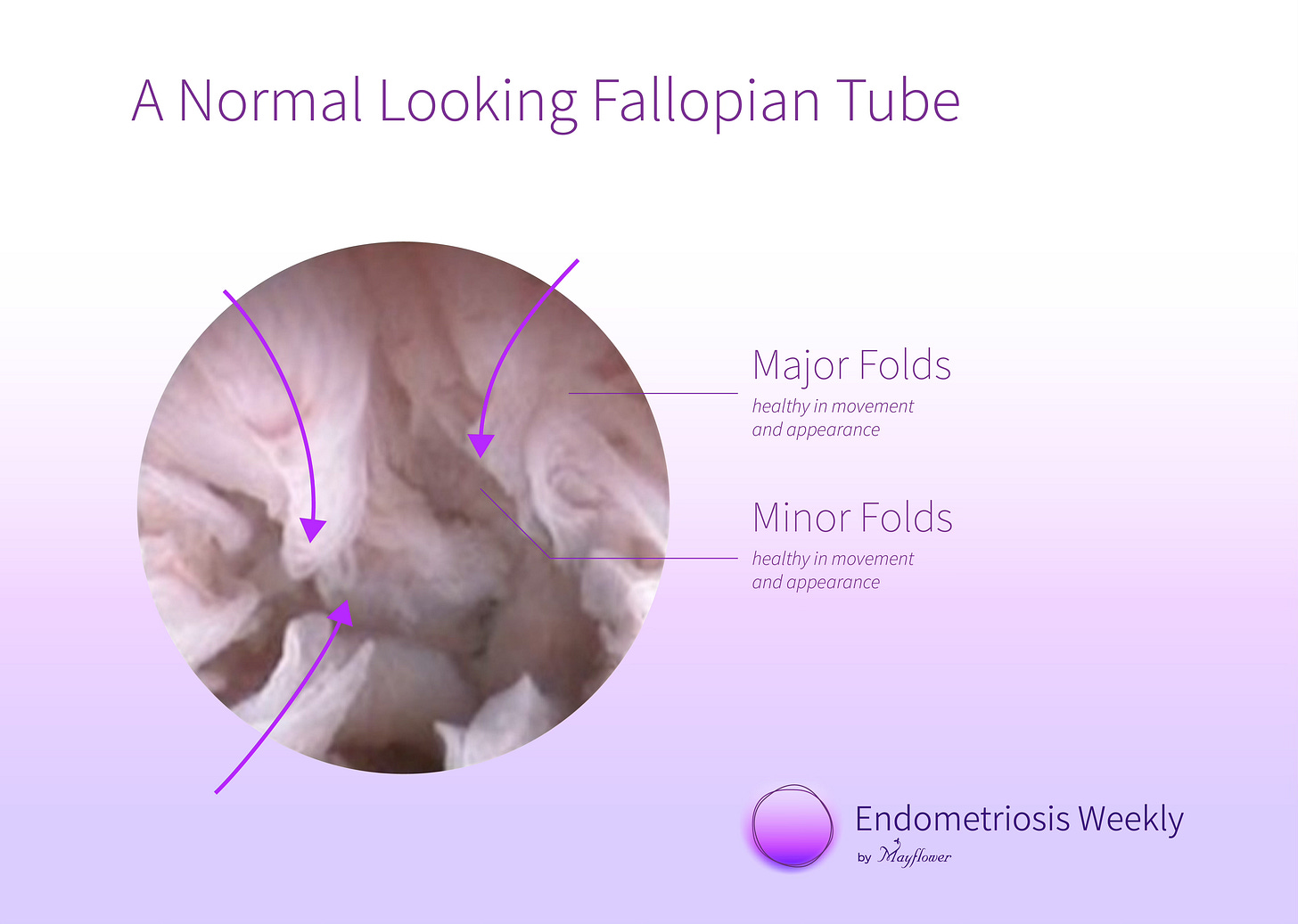
Of course, you’re never going to know what’s wrong with the world till someone shows you what’s right. So we begin by looking at the state of a healthy interior lining of the fallopian tube.
Observe that there are some major folds, that are large and radiating inwards, and then there are some minor folds, that are shorter and interspersed between two major folds. It’s the nature of these folds and their staining patterns with a methylene blue dye that will help us grade them.
Let’s now begin looking at degraded tubes in ascending order
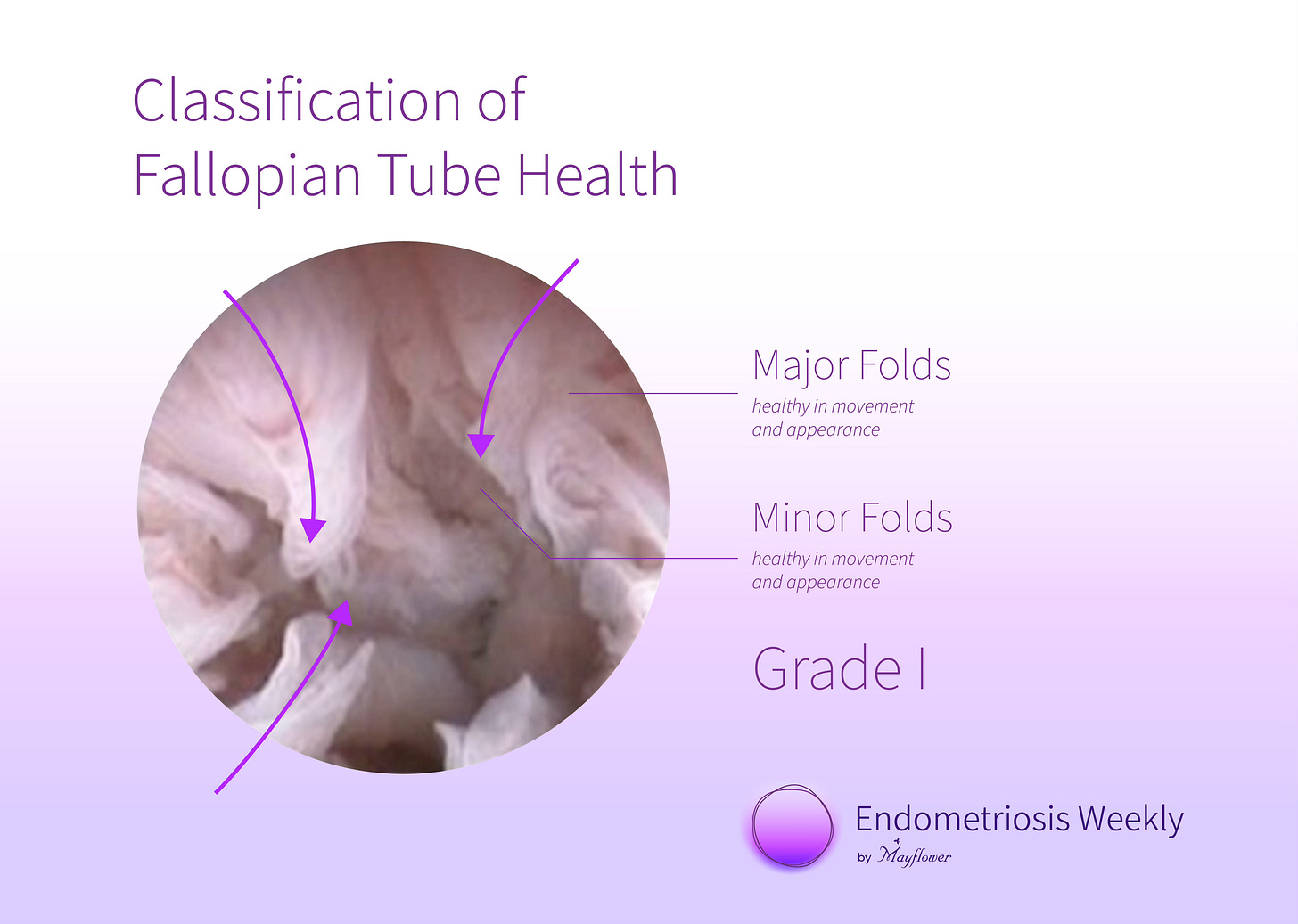
Grade 1
For categorisation purposes, this is the same as a healthy tube.
Major folds look healthy and normal
Minor folds look healthy and normal
These folds can trap the egg and move it forward towards the isthmus of the tube and at the same time, facilitate the movement of sperm from the isthmus towards the ampula. They facilitate both a progressive as well as and controlled movement of gamets from and into the uterus.
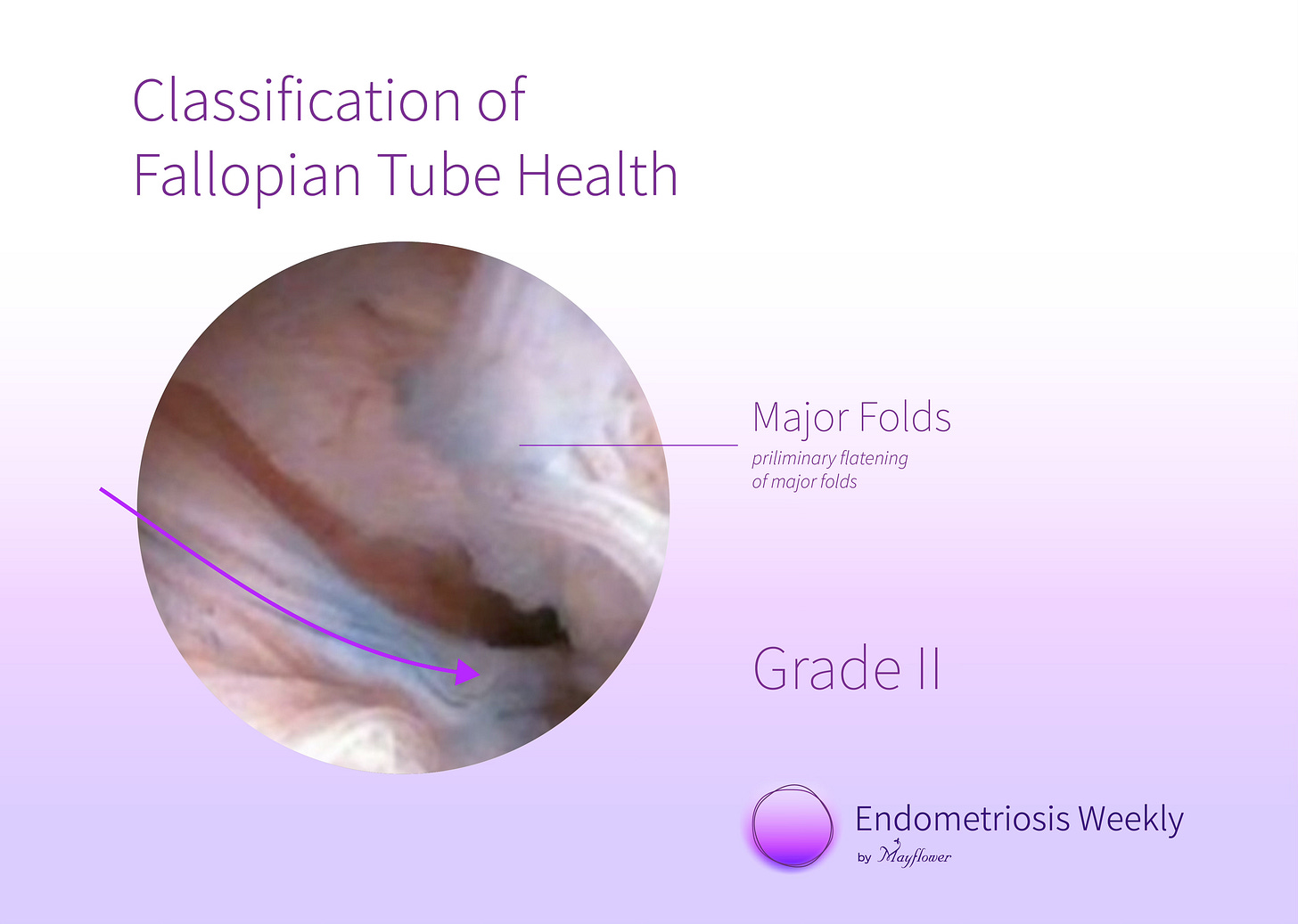
Grade 2
A second-grade fallopian tube is characterised by some initial damage to the lining of the tube. The major folds are separated and minimally flattened but otherwise the tube appears to be healthy.
Some nuclear staining of the mucosa might also be observed.
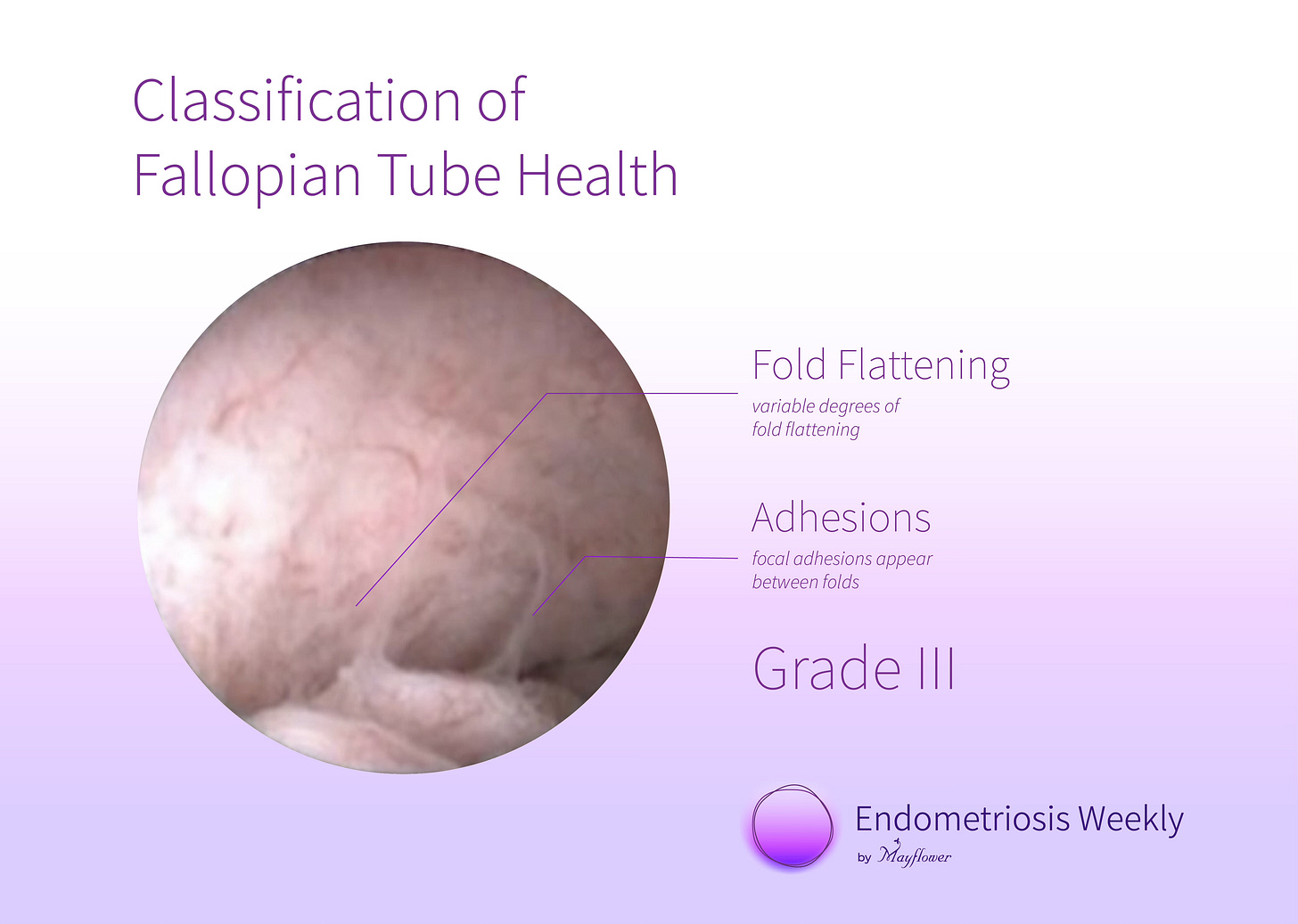
Grade 3
This is when things start to get complicated. A typical appearance of a grade 3 salpinx shows a variable degree of fold flattening with focal adhesions between mucosal folds.
Some could say that grade 3 is an early detection of a blocked tube, however, chances of natural conception rapidly dwindle beyond this point.
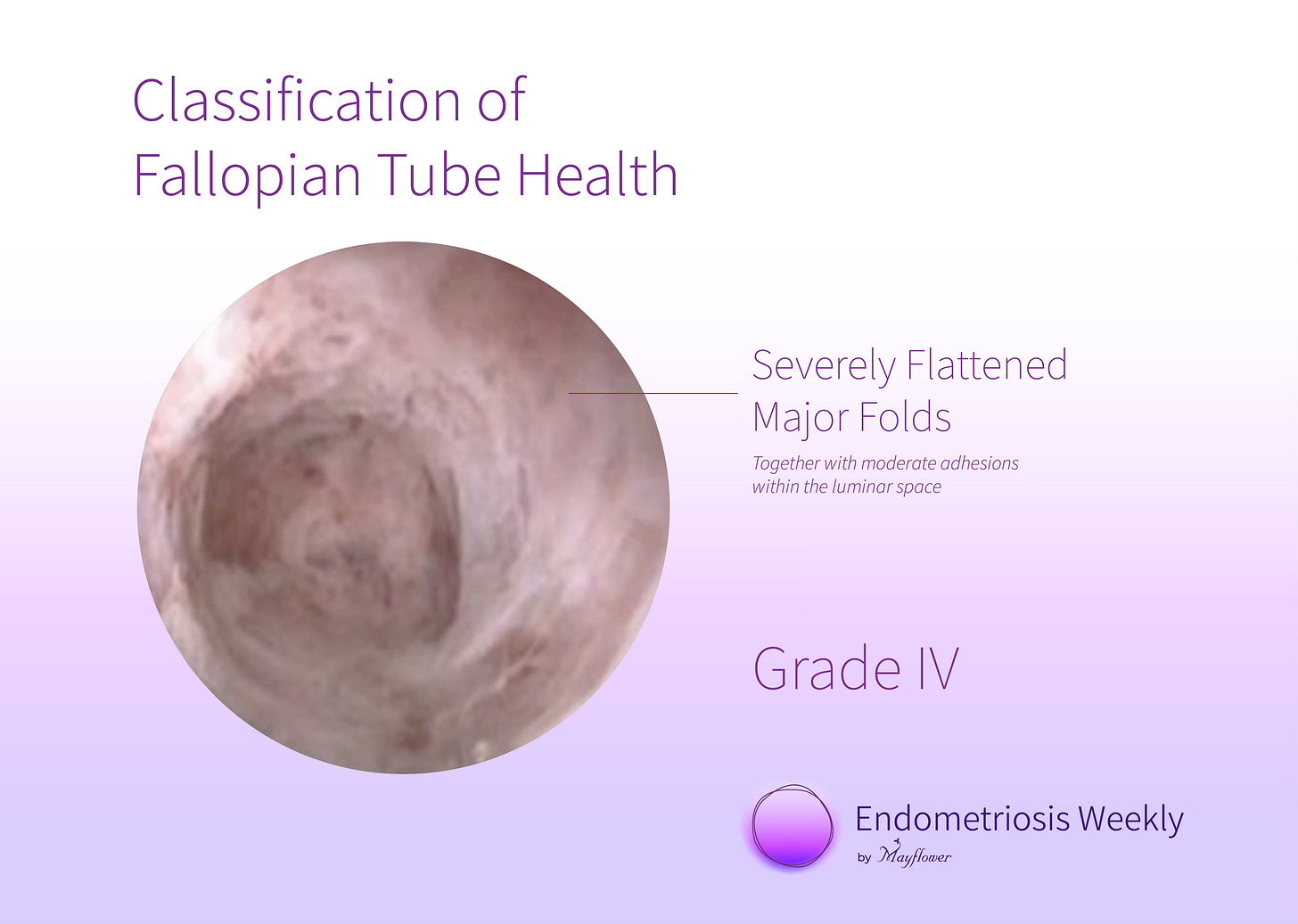
Grade 4
This grade is characterised by severe flattening of the folds and a moderate degree of adhesions. This is when a tube might still appear somewhat normal in an HSG but in reality, has lost its ability to harbour gametes and move them from one point to the other.
The core function of the fallopian tube now becomes very clear. It is not simply a passive tube from which the gametes move but it indeed serves a much more critical function.
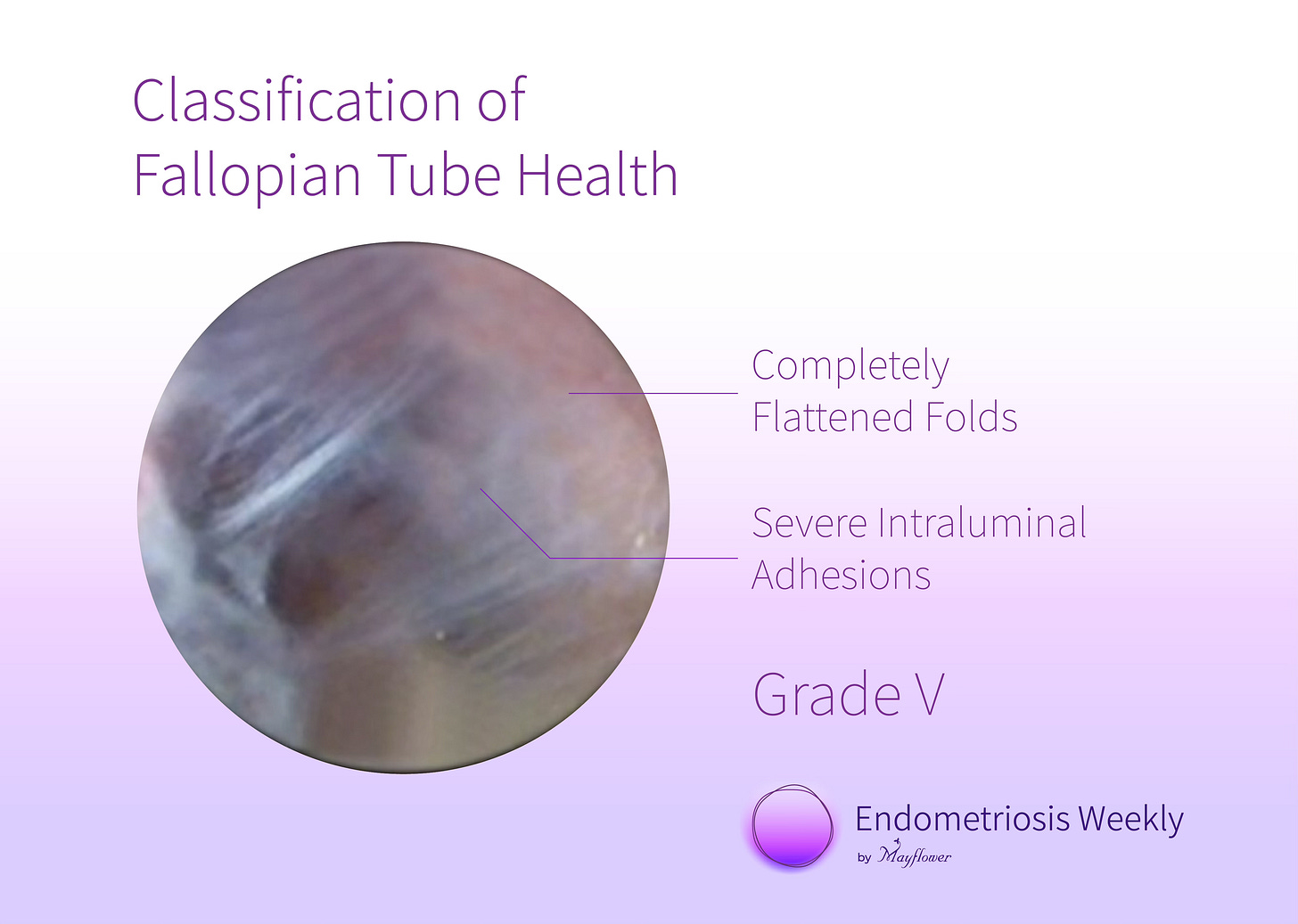
Grade 5
This is when both the patency and permeability of the salpinx are lost. The folds are completely flattened and severe intraluminal adhesions lead to a total loss of endothelial architecture.
Understandably, the likelihood of natural conception is extremely low given the conducting and harbouring potential for the salpinx is significantly lost.
In grades 1, 2, and 3, the salpingoscopy procedure’s pressurised fluid injection leads to some degree of improvement in tubal permeability. While this correlation hasn’t directly been studied, we’ve observed a strong improvement in natural conception rates amongst women who underwent the procedure after presenting with infertility.
It is clear that in grades 2 and 3 where the impact on tubal function is intermediate, a salpingoscopy procedure was observed to be followed by a significant occurrence of natural conception.
In cases that did not see success here, IVF remains an option where ovarian health (AMH reserves), uterine health, and other factors become important considerations, all of which typically get assessed anyway in pre-op diagnosis for infertility.
In conclusion, an accurately assessed and astutely performed salpingoscopy procedure has a significant likelihood of helping fertility without causing any major anatomical trauma. In that sense, it is a powerful weapon in the armoury of an infertility specialist.
That’s it for this week. Please don’t forget to leave your thoughts in your reply. We love reading all your emails! For those reading this online, you can write to us at ew@mayflowerhospital.com







Earlier we used to see the patency of the Tubes and hoped for good outcome; now that the function of the tubes is added with advanced technology the results have improved.
Thanks to the advanced technology which is helping the patients
Dr Pushpa Srinivas